Archives
Exclusive: Croydon University Hospital hires ‘£5,000 per day’ QC to fight tribunal’s damning whistleblower’s verdict
Croydon Advertiser | Posted: January 14, 2015

Jane McNeill QC has been instructed by Croydon University Hospital to help appeal Dr Kevin Beatt’s (centre) tribunal verdict. Chief executive John Goulston, right, declined to be interviewed this week
He won his case in October after a judge decided he had been sacked for raising concerns following the death of a patient during a routine operation in 2011, rejecting the hospital’s claim he had been guilty of gross misconduct.
The hospital continues to reject the tribunal’s damning judgement and has instructed a top QC to work on an appeal alongside the barrister already working on the case, the Advertiser can reveal.
Leading silk Jane McNeill QC, of Old Square Chambers, commands between £50,000 to £60,000 to prepare a case up until the first day of a hearing and between £4,000 to £5,000 per day thereafter. Ian Scott, a junior also from Old Square, represented the trust at the tribunal.
Tony Newman, leader of Croydon Council, has called on the hospital to “take a long hard look” at whether the spending is appropriate.
Gavin Barwell, MP for Croydon Central, said: “I will need to speak to the hospital, but at first sight I think my constituents will question whether, given the undeniable pressure the NHS is under, the hospital should be spending these sums of money on an employment tribunal, particularly when there has been a clear verdict.”
Hospital becomes first in London to declare major internal incident due to A&E demand.
Croydon Health Services said chief executive John Goulston was unavailable for interview when approached by the Advertiser this week.
Instead it provided a written statement in which it stood by its reasons for sacking Dr Beatt and did not respond to any questions about Ms McNeill or its legal expenditure.
According to figures provided to the Advertiser via a Freedom of Information request, the trust had spent £132,048 on the case as of December 11, including all solicitor and counsel fees since Dr Beatt submitted his claim after being sacked in September 2012.
He had alleged one of his patients, Gerald Storey, had died because a nurse had been suspended without his knowledge, meaning she was unable to help him during the procedure.
After informing the coroner and a senior GP the trust sacked him for gross misconduct, claiming his account was “unsubstantiated” and made to “serve an ulterior motive”.
Those claims were rejected by the employment tribunal which found Dr Beatt, 63, raised “genuine” concerns – later substantiated by the coroner – only to be dismissed because he was a whistleblower.
The tribunal’s lengthy report was highly critical of senior managers at the hospital, including Mr Goulston and Michael Parker, then the trust’s chairman.
It alleged that one of Dr Beatt’s colleagues – Dr Asif Qasim – was a bully and that he and another manager had pressured witnesses to change their statements about what had happened on the day of Mr Storey’s death.
Speaking to the Advertiser this week, Dr Beatt said the final cost of the legal proceedings will far exceed the £132,048 bill the trust has accrued so far. The hospital should learn whether it has been given leave to appeal – or even go to a full re-hearing – within the week.
Dr Beatt said: “The hospital is spending huge amounts of public money, not to defend the trust or the clinical service, but to defend the reputation of its managers.
“The NHS has this vast budget and there’s no accountability for how managers spend it. This couldn’t apply in any other business where this amount of money would be at stake.”
Cllr Newman said: “Having looked closely at this case, at a time when the NHS is under huge financial pressure, and its A&E is in crisis, I would ask the hospital to take a long hard look at whether spending tens of thousands of pounds, that the NHS does not have, on this issue, is the best use of the hospital’s budget.”
A Croydon Health Services spokesman said: “It is every employee’s responsibility at Croydon Health Services to uphold great care for our patients and we take all concerns raised extremely seriously.
“Dr Beatt was not dismissed for whistleblowing and we stand by our reasons for dismissal. We have investigated his claims thoroughly.
“The trust is appealing the decision of the Employment Tribunal and we will not be commenting further on this matter until these legal proceedings are complete.”
Quality of care and patient safety in the UK: the way forward after Mid Staffordshire
By Brian Jarman
Dr Foster Unit, Imperial College Faculty of Medicine,
London EC4Y 8BN, UK
In the past decade, quality of care and patient safety in British hospitals have become the focus of increasing public, professional, political, and regulatory concern. The 2001 inquiry into paediatric cardiac surgery at Bristol Royal Infirmary concluded that the Department of Health was unable to respond to an issue of quality of care, even though the Department of Health accepted that ultimate responsibility rests with it and the Secretary of State for Health.1 The Bristol Royal Infirmary Inquiry warned that quality of care problems could recur in the National Health Service (NHS) in future. After the recommendations of an external investigation of Bristol were implemented, the adjusted death rate at the paediatric cardiac surgery unit dropped from 29% to 3% within 3 years.2 The families of children who underwent cardiac surgery at Bristol should have been told of the lower mortalities at other units.
In 2001, the Dr Foster company published the first of their annual Good Hospital Guides in UK national newspapers: these included hospital standardised mortality ratios (HSMR).3–5 The HSMR is the ratio of the number of observed deaths in a hospital over a certain time to the number that would be expected if the hospital had the national death rate accounting for the adjustment factors, such as age, sex, diagnosis, and emergency admission. Although it has limitations, the HSMR is a trigger to ask hard questions and understand where performance may be falling short. Since 2003, the Dr Foster website also reported monthly mortality alerts6 for particular diagnoses or procedures for NHS organisations and professionals. From April 2007, these alerts were sent by letter from Imperial College London to the chief executives of any English NHS hospital trust that was found to have a risk-adjusted death rate for a particular condition that was double the national rate in the preceding 3 months, and the chance of it being a false alarm was less than 1 in 1000. The letters were copied to the hospital regulator, the Healthcare Commission (and now to its successor the Care Quality Commission [CQC]).
In 2007, when the Mid Staffordshire General Hospitals NHS Trust was supported by its oversight Strategic Health Authority for Foundation Trust status, its HSMR published in the Good Hospital Guide was the fifth highest of English acute trusts.3 The Department of Health cautioned the public against using HSMRs to judge the relative safety of hospitals.7 The Department of Health was not informed of the high HSMR or mortality alerts at Mid Staffordshire when they agreed, in June, 2007, to approve the trust’s application to Monitor, the Foundation Trust regulator, for final approval.8 Monitor was told by the trust that Mid Staffordshire’s apparently high HSMR was an artifact of coding.8 David Nicholson, initially Chief Executive of the Strategic Health Authority and later of the NHS, said the data that were available to the regulators did not indicate a problem at Mid Staffordshire,9 even though the trust had logged on and seen its mortality alerts 847 times.10 Nicholson considered Mid Staffordshire “singular” and not illustrative of a systemic problem, an attitude described by the Mid Staffordshire NHS Foundation Trust Public Inquiry Counsel as very dangerous and not supported by evidence to the Inquiry.11 The trust is now considered by Monitor to be neither clinically nor financially sustainable.12
Robert Francis’ inquiry into the problems at, and regulation of, Mid Staffordshire NHS Foundation Trust found a widespread culture of denial, and he, his Harvard experts, and Bruce Keogh, Medical Director of the NHS, all considered that monitoring HSMRs had provided grounds for investigating the trust.8,13 The Department of Health chief analyst suggested it was a “system failure” not to have done so, and Keogh agreed that problems at Mid Staffordshire would have been spotted earlier by the Department of Health had that happened.8 The Francis report documented the appalling care received at that trust8 and as a result the Prime Minister David Cameron asked Keogh to investigate the 14 trusts with the highest death rates.14 Keogh’s report found that none of the trusts could be given a clean bill of health and action plans were produced for each.14 The Secretary of State for Health Jeremy Hunt announced that 11 of the trusts would be placed into special measures for fundamental breaches of care.15 The HSMRs of 11 of the trusts had been identified in the 2007 Dr Foster Good Hospital Guide as significantly high, including ten of the 11 that were placed into special measures in 2013.3,15 I notified seven of the 14 hospitals to the then Secretary of State for Health in 2010 and he referred them to the CQC.10 However, individual cases of clinical quality were, and are, not investigated by the CQC or the Health and Safety Executive; the NHS has no investigator of poor clinical care. That is a regulatory gap that should be closed.8
As with the Bristol Royal Infirmary, the national systems for ensuring quality and patient safety had failed at Mid Staffordshire and nationally. Why did that happen? Before the Bristol Royal Infirmary Inquiry there were systems in place that dealt with performance management and clinical outcomes,10 and after Bristol there were great promises16 with the formation of the National Patient Safety Agency (NPSA) and the Commission for Health Improvement (CHI), which detected the problems at Mid Staffordshire in 2002.8 However, between 2003 and 2004 things went wrong. Ian Kennedy referred to what Gordon Brown described in a 2005 speech as a “bonfire of the regulators”.17 CHI was abolished and replaced by the Healthcare Commission, which was slow to detect the appalling events at Mid Staffordshire.8,18 The NPSA acknowledged significant under-reporting of safety incidents18 and was abolished, with its functions incorporated into the CQC. The Independent Review Panels that investigated patients’ complaints about hospital services not resolved at the hospital were abolished, and in 2011–12 only one of 375 written hospital complaints had been formally investigated by the Ombudsman.19 The independent Community Health Councils were abolished in 2003. During the Mid-Staffordshire Public Inquiry, the chairmen of the three main health-care regulators commented on the difficulties they faced. Ian Kennedy, of the Healthcare Commission, stated: “The engagement of the Department of Health was one of interest… quality of the care provided by the NHS was not part of their agenda.”20 Barbara Young, of the CQC, stated: “The reason the government didn’t like tough reports was because they were running the services that were being reported upon.”21 William Moyes, of Monitor, stated: “The culture of the NHS, particularly the hospital sector, I would say, is not to embarrass the minister.”22 The then Minister Andy Burnham said “The impression of us all was that we would just, you know, constantly do what was meant to be the thing that Number 10 wanted or that we were all, you know, unthinkingly piling this stuff through. We weren’t.”23
Since the publication of the Francis Report8 things are changing. The CQC Chairman, Chief Executive, and most of the Board have been changed and, with the Chief Inspector of Hospitals for England, the CQC will undertake thorough inspections in future using trained, professional investigators.24 The Parliamentary Health Service Ombudsman has called for improvements in the way hospital complaints are handled and said that she will formally investigate ten times as many patient complaints.25 There is an intention to abolish the widespread so-called gagging clauses that undermine the culture and transparency of the NHS.26 Francis has recommended a statutory obligation to observe a duty of candour for health-care providers and registered medical and nursing practitioners, and a criminal offence for non-compliance.8 However, as Don Berwick’s recent report on patient safety for the Department of Health makes clear, it is important that this judicial intent does not lead to punishing or criminalising clinicians for unintentional mistakes or involvement in failed systems.27 The existing criminal law can deal with bad cases. Continuous learning and improvement,28 monthly mortality alerts, adjusted death rates,8,27 regular patient and staff feedback, and targeted, skilled hospital investigations could lead to a safe NHS, ideally without a culture of denial8 or gagging clauses.
To improve the quality of care in UK hospitals I would reintroduce the Independent Review Panels and Community Health Councils and develop monthly complaints alerts similar to the mortality alerts. Regulation would be more independent if the CQC reported in public to Parliament, and there would be better communication if it were integrated with Monitor. Additionally, it is important to ensure there are minimum staff-to-patient levels12 of doctors and nurses, with 65% trained nurses3 and regulation of health-care assistants. I would aim for total physicians per head of population at the EU average.29 Ideally I would also like to see training introduced for the boards of trusts and for them to have equal representation of patients, clinicians, finance, and managers. There has been a decade of concerns about the quality of care in our hospitals: patients have been ignored, the regulatory systems have failed, and there has been a culture of denial. With political will the proposed reforms could lead to marked improvements.
I am employed part-time as the Director of the Dr Foster Unit at Imperial College London. I am paid a consultancy fee by Dr Foster Intelligence for my international work on advice and involvement with development of international relations and am paid as a part-time Senior Fellow at the Institute for Healthcare Improvement in Cambridge, MA, USA.
1 The Bristol Royal Infirmary Inquiry. Learning from Bristol: the report of the
public inquiry into children’s heart surgery at the Bristol Royal Infirmary
1984–1995. July 2001. CM 5207. London: Stationery Office, 2001.
2 Aylin P, Bottle A, Jarman B, Elliott P. Paediatric cardiac surgical mortality in
England after Bristol: descriptive analysis of hospital episode statistics
1991–2002. BMJ 2004; 329: 825.
3 Dr Foster Intelligence. Dr Foster April 2007 Good Hospital Guide. http://
drfosterintelligence.co.uk/wp-content/uploads/2011/06/The-Hospital-
Guide-2007.pdf (accessed Aug 8, 2013).
4 Jarman B, Gault S, Alves B, et al. Explaining differences in English hospital
death rates using routinely collected data. BMJ 1999; 318: 1515–20.
5 Bottle A, Jarman B, Aylin P. Strengths and weaknesses of hospital
standardised mortality ratios. BMJ 2011; 342: c7116.
6 Bottle A, Aylin P. Intelligent information: a national system for monitoring
clinical performance. Health Serv Res 2008; 43: 10–31.
7 Martin N. Revealed: lottery of death rates in hospitals. The Telegraph,
April 24, 2007. http://www.telegraph.co.uk/news/uknews/1549493/
Revealed-Lottery-of-death-rates-in-hospitals.html (accessed Aug 8, 2013).
8 The Mid Staffordshire NHS Foundation Trust. Public Inquiry Chaired by
Robert Francis QC. Report of the Mid Staffordshire NHS Foundation Trust
Public Inquiry. 3 vols. London: Stationery Office, 2013. http://www.
midstaffspublicinquiry.com/report (accessed Aug 8, 2013).
9 Hansard. The Health Committee, HC 982–ii. House of Commons, page 22.
Report of The Mid Staffordshire NHS Foundation Trust Public Inquiry.
March 5, 2013. Sir David Nicholson KCB CBE, question Q203. http://www.
publications.parliament.uk/pa/cm201213/cmselect/cmhealth/uc982-ii/
uc98201.pdf (accessed Aug 8, 2013).
10 Mid Staffordshire NHS Foundation Trust Public Inquiry. June 13, 2013.
Statement of Sir Brian Jarman. Paragraphs 25–27. http://www.
midstaffspublicinquiry.com/sites/default/files/evidence/Brian_Jarman_-_
witness_statement.pdf (accessed Aug 8, 2013).
11 Mid Staffordshire NHS Foundation Trust Public Inquiry. Oral hearings. Dec 1,
- Page 193, lines 5–6. http://www.midstaffspublicinquiry.com/sites/
default/files/transcripts/Thursday_1_December_2011_-_transcript.pdf
(accessed Aug 8, 2013).
12 Monitor. Monitor—contingency planning team, Mid Staffordshire NHS
Foundation Trust, assessment of sustainability, January, 2013. http://www.
monitor-nhsft.gov.uk/sites/default/files/publications/MSFT%20
Sustainability%20Final.pdf (accessed Aug 8, 2013).
13 Robert Francis, QC. Notes for presentation of letter to SoS submitting Mid
Staffs Independent Inquiry. Feb 5, 2010. http://www.midstaffsinquiry.com/
assets/docs/Report-presentation-by-Robert-Francis-QC.doc (accessed
Aug 8, 2013).
14 Keogh B. Review into the quality of care and treatment provided by
14 hospital trusts in England: overview report. July 16, 2013. London:
NHS England, 2013. http://www.nhs.uk/NHSEngland/bruce-keoghreview/
Documents/outcomes/keogh-review-final-report.pdf (accessed
Aug 8, 2013).
15 Hansard. House of Commons. Hospital mortality rates. July 16, 2013.
Column 927. http://www.publications.parliament.uk/pa/cm201314/
cmhansrd/cm130716/debtext/130716-0001.htm#13071683000004
(accessed Aug 8, 2013).
16 Department of Health. An organisation with a memory. London: Stationery
Office, 2000.
17 Mid Staffordshire NHS Foundation Trust Public Inquiry. May 4, 2011.
Oral evidence of Sir Ian Kennedy, day 77. Page 33, lines 3–23. http://www.
midstaffspublicinquiry.com/sites/default/files/transcripts/Wednesday_4_
May_-_transcript.pdf (accessed Aug 8, 2013).
18 House of Commons. Patient Safety Health Committee. Measurement and
evaluation, paragraph 36. http://www.publications.parliament.uk/pa/
cm200809/cmselect/cmhealth/151/15106.htm (accessed Aug 8, 2013).
19 Jarman B. Professor Brian Jarman guest editorial: not many complaints are
investigated. nhsManagers.network, May 14, 2013. http://www.
nhsmanagers.net/guest-editorials/not-many-complaints-are-investigated/
(accessed Aug 8, 2013).
20 Mid Staffordshire NHS Foundation Trust Public Inquiry. April 4, 2011.
Witness statement of Sir Ian Kennedy, paragraph 39. http://www.
midstaffspublicinquiry.com/sites/default/files/evidence/Sir_Ian_Kennedy_-_
witness_statement.pdf (accessed Aug 8, 2013).
21 Mid Staffordshire NHS Foundation Trust Public Inquiry. Oral hearings,
day 110. July 4, 2011. Page 74, line 20. Page 75, line 9. http://www.
midstaffspublicinquiry.com/sites/default/files/transcripts/Monday_4_
July_2011_-_transcript.pdf (accessed Aug 8, 2013).
22 Mid Staffordshire NHS Foundation Trust Public Inquiry. Oral hearings,
day 93. June 1, 2011. Page 11, line 24. Page 12, line 1. http://www.
midstaffspublicinquiry.com/sites/default/files/transcripts/Wednesday_1_
June_2011_-_transcript.pdf (accessed Aug 8, 2013).
23 Mid Staffordshire NHS Foundation Trust Public Inquiry. Oral hearings,
day 115. Sept 6, 2011. Page 138, lines 2–5. http://www.
midstaffspublicinquiry.com/sites/default/files/transcripts/Tuesday_6_
September_2011_-_transcript.pdf (accessed Aug 8, 2013).
24 Care Quality Commission. Consultation on changes to the way we inspect,
regulate and monitor care services. July, 2013. http://www.cqc.org.uk/
public/sharing-your-experience/consultations/consultation-changes-waywe-
inspect-regulate-and-monito (accessed Aug 8, 2013).
25 Donnelly L. Ombudsman: patients suffer from a “toxic cocktail” in NHS.
The Telegraph, Aug 12, 2013. http://www.telegraph.co.uk/health/
healthnews/10238221/Ombudsman-Patients-suffer-from-a-toxiccocktail-
in-NHS.html (accessed Aug 13, 2013).
26 Hammond P. The NHS is still not safe for whistleblowers. The Times,
March 15, 2013. http://www.thetimes.co.uk/tto/opinion/thunderer/
article3713910.ece (accessed Aug 8, 2013).
27 National Advisory Group on the Safety of Patients in England. A promise to
Call for evidence: NHS complaints and clinical failure

Public Administration Select Committee (PASC) invites written evidence on the issue of NHS Complaints and Clinical Failure, ahead of oral evidence sessions early in the new year.
PASC launches a new inquiry into how incidents of clinical failure in the NHS are investigated – and how subsequent complaints are handled. The Committee is considering ways that untoward clinical incidents could be investigated immediately at a local level, so that facts and evidence are established early, without the need to find blame, and regardless of whether a complaint has been raised. It is hoped that this work will reduce the need for complaints to go to the Parliamentary and Health Services Ombudsman (PHSO), whose main role relates to administrative and service failures in the NHS in England.
The inquiry aims to
- examine the effectiveness of existing approaches to investigating and addressing systemic safety issues currently present within the NHS
- explore the relative benefits that a new clinical accident investigation body might bring to this area and how analysis of complaints could inform its work
- consider models of best practice within other sectors and examine their transferability to the healthcare sector; and to
- explore the role that the PHSO might play in the functioning of any new accident investigation body
PASC would like to hear views on
- The effectiveness of the NHS’s current approach to investigating and addressing untoward medical incidents.
- How lessons about best practice, procedures and human factors should be learned and disseminated.
- The value that a new, single, clinical accident investigation branch of the Department of Health would bring to the healthcare sector and how this could improve the complaints process.
- The current capacity of the PHSO to manage and investigate complaints relating to clinical incidents, and their ability to analyse and assess medical evidence.
- The impact that Department of Transport accident investigation branches have had in the transport sector and the lessons that have been learnt from the establishment and use of such bodies, in the UK and in healthcare systems in other countries.
- How any such body within the healthcare sector would support the work of PHSO.
- The legal drivers behind increased challenges associated with the issue of medical liability, and the failure to address clinical incidents and complaints.
Bernard Jenkin MP, Chair of the Committee, said
“It is very unfortunate that the way clinical failures – which can be a tragedy for a person and their loved ones – are handled by the NHS and its watchdogs does not seem to foster positive outcomes or learning from mistakes that have been made. There seems to be a culture of blame and of responding only to complaints, rather than an environment where clinicians can come forward and lay out the facts of things that have gone wrong, or express concerns, so that they can be investigated and lead to improvements. Right now the only outcomes after clinical failings seem to be another excoriating report by a health watchdog, litigation or the passing of badly handled complaints further up the chain to adjudicators of last resort like the PHSO, which reports to Parliament through PASC. These outcomes may be the result of ‘starting from the wrong place’. We would like to examine the possibilities of new ways of reporting and investigating clinical failures that could being about positive outcomes and change at a much earlier stage. We are interested in the experience in other countries, particularly in New Zealand, which drew the support of a 2009 Health Select Committee Report on Patient Safety.”
The Committee would also welcome views on any other matters that may be relevant to this inquiry. Please do not feel obliged to respond to all of the questions if you have a specific interest.
Recent developments
Work in this area has been prompted by public debate and the recent publication of an article in the Journal of the Royal Society of Medicine by Carl Macrae (Centre for Patient Safety and Service Quality, Imperial College London) and Charles Vincent (Department of Experimental Psychology, University of Oxford). This article compares accident investigation within the healthcare sector to that within air, rail and maritime transport. It argues that whilst these industries are “served by an independent and permanently staffed organisation that is explicitly charged with investigating serious safety risks and major failures”, no similarly consistent approach exists within the NHS:
“These independent investigators are responsible for coordinating all major safety investigations in their industry. They have a remit to investigate the entire industrial complex, encompassing design of equipment, the culture and practices of delivery organisations such as airlines or shipping companies, and the role of regulators and government. Their independence is essential to their effectiveness. It allows them to routinely investigate the full range of factors that underlie major failures, irrespective of whether those are rooted in the behaviour of an individual professional or the design of an entire regulatory system.”
Macrae and Vincent suggest that by applying such learnings the NHS could develop an investigation agency for healthcare which would be:
- Independent and impartial. No executive, regulatory, commissioning or performance management functions
- Transparent. Clear, timely, open communication of findings of investigations, recommendations and monitoring of implementation
- Established as permanent body able to investigate and follow up recommendations over years
- Collaborative and cooperative. Working in partnership with those being investigated
- Authority to access all sites, organisations, staff and information across the healthcare system
- Non-punitive. Separated from assignment of blame or liability and legally protected
- Accountable
Background
PHSO investigates complaints where individuals have been treated unfairly or have received poor service from government departments, other public organisations and the NHS in England. The service that PHSO provides is governed by law, free to use, open to everyone and completely independent.
PASC scrutinises the reports of the Parliamentary and Health Service Ombudsman. PASC monitors complaints about the Ombudsman as a way of examining the work of her office and identifying systemic problems, but does not consider individual cases.
How to respond
- Responses should be submitted by noon on Friday 16 January 2015 through the inquiry page.
- Guidance on written submissions
2014 accountability hearing with CQC
HOC HEALTH COMMITTEE Tuesday 16 December 2014
|
Committee Room 15 2014 accountability hearing with the Care Quality Commission Witnesses Charlotte Leslie – questioning on whistleblowing 16.08.19 mins into the following video http://www.parliamentlive.tv/Main/Player.aspx?meetingId=16821 |
Care Quality Commission: Fiddling while whistleblowers burn?
By Minh Alexander, Redundant whistleblower, Consultant Psychiatrist 1999 to 2013 27 December 2014
The CQC is an arms length body of the Department of Health, accountable to The Secretary of State for Health, who must account to Parliament. Procedurally, the CQC must align itself with Department of Health (DH) strategy[1].
What does CQC behaviour say about DH strategy regarding whistleblowers?
The CQC has been well known to chant to whistleblowers seeking help and protection, the DH mantra: “It’s an employment issue”.
On 22 December 2014 a CQC Non Executive Director tweeted, albeit in a personal capacity:
“At the moment, it is an HR/employment issue. Unsure how this can change tbh”.
When a whistleblower commented that it was scandalous that CQC seemed to have no role in protecting whistleblowers, that person was accused thus by this CQC Non Executive Director:
“If you twist words & attack, you damage the cause”
When I opined that the “HR/employment” comment was very alarming, and that poor HR governance and whistleblower suppression were patient safety issues, I too received a similar response:
“You are twisting my words – unhelpful. This is behaviour that needs to stop…”
The CQC has a history of poor HR governance, and of a bullying culture. In my view its ineptitude in handling whistle blowing, both by its own staff and by staff from the bodies that it regulates, has been clear.
In 2011 I wrote to the CQC to question the fact that it had no published policies on whistle blowing. It seemed to me that this dearth of written commitments was a natural extension of the CQC’s poor values and attitudes to whistle blowing, and to whistleblowers.
So, have things changed under the new the CQC regime?
When Raj Mattu and colleagues whistle blew to the CQC’s predecessor body in 2001, it “mystifyingly” passed their names to the Trust’s CEO.[2] Raj subsequently endured a decade of catastrophic persecution, including countless complaints about him to the GMC.
Fast forward to the present. In November 2014, veteran whistleblower Shiban Ahmed passed dossier to the CQC about 22 cases of unsafe circumcision, and expressed concerns that the CQC had not done enough previously about his disclosures. In response, a CQC inspector copied an email about his disclosure to his employer. Shiban has since been suspended and referred to the GMC.[3]
Not a lot of change evident there then.
Perhaps the CQC should reflect on the degree to which its activities trigger whistle blower persecution, and its responsibility for severe detriment and suffering that follow.
No apology from the CQC is apparent for what has happened to Shiban, or the fact that very unsafe circumcisions of children continue, despite his repeated disclosures. Instead, there is a carefully worded denial:
“The CQC has not reported Mr Ahmed to the GMC or to his trust and has not invoked any disciplinary action against him”
When faced with pressure to protect a whistleblower, a CQC response may include protestation that it has no legal powers to do so. I have personal experience of this particular CQC rebuttal.
On the matter of the CQC’s powers, the above CQC Non Executive Director tweeted on 22 December 2014:
“You need a legal basis. Otherwise no point”.
Whilst the CQC’s claim that it has no formal powers to protect whistleblowers is arguable, we all know that a great deal is done by influence. Early in my journey, a supportive and effective CQC inspector protected me. I know it can be done, and it should be a model for CQC practice.
However, the mayhem often starts when the CQC turns a blind eye, fails to respond appropriately to whistleblowers’ disclosures, and claims that it has no jurisdiction to protect. Washing of regulatory hands can be a green light for whistle blower suppression and victimisation.
Continuing, un-rectified, gross injustices to whistleblowers, and failures by the CQC to act appropriately, light up that particular neon beacon. Homelessness, grave illnesses and financial ruin are poor reward for dedication. Whistleblowers are also still forced to make disclosures through the media.[4]
Despite the new CQC regime’s claims that it would be more responsive to concerns, and that it would operate more transparently, an FOI enquiry forced the CQC to admit, on 17 June 2014, that it had undertaken no “central analysis” of the reasons behind 981 whistleblower disclosures, received in the preceding 12 months.[5] When I recently asked the CQC if it would carry out an analysis and publish it, the CQC did not answer the questions straightforwardly. Instead, it said my enquiry would also be dealt with as an FOI request. Will the CQC meet the fast approaching deadline for disclosure 29 December 2014, or will it tarry?
Transparency is also lacking in the CQC’s failure so far to publish its evidence to Sir Robert Francis’ review on whistle blowing. In an interesting form of words, the CQC stated in its December 2014 report, “Complaints Matter”, that it would publish a “fuller account” of its activities when Sir Robert publishes. [6] However, I have received no response from David Prior (CQC Chair), to several requests for the CQC to clarify if this means that CQC will publish all of the evidence that it has submitted to Sir Robert.
I can see no valid or credible reason for organisations’ submissions to the Speak Up review remaining confidential. Opacity serves only to avoid constructive challenge and scrutiny. Is the CQC’s failure to publish its evidence a symptom of unaccountability, and image management, by a “comfort-seeking” organisation? [7]
“Comfort-seeking behaviours are defined here as being focused on external impression management and seeking reassurance that all was well; consequently, what was available to organisations was data, but not intelligence. Serious blind spots could arise when organisations used a very limited range of methods for gathering data, were preoccupied with demonstrating compliance with external expectations, failed to listen to negative signals from staff or lacked knowledge of the real issues at the frontline. Comfort-seeking tended to demonstrate preoccupation with positive news and results from staff, and could lead to concerns and critical comments being dismissed as ‘whining’ or disruptive behaviour”.
The CQC asserted in “Complaints Matter” that it had consulted whistleblowers about its handling of concerns. However, this was based on focus group data. No information was given about methodology and numbers. Tellingly perhaps, the CQC has not responded to questions about whether it will arrange transparent, independent audit of whistleblowers’ experience of its handling of their concerns.
The CQC’s joint investigation with Monitor into the reported dysfunctional culture at the Christie, [8] did not support the concerns of several whistleblowers. This does not bode well for the CQC’s application of FPPR in relation to whistleblower suppression.
In my view, the altruism and commitment of whistleblowers, some who lose their careers, their livelihoods, their health and family life, does not seem matched by suitably principled behaviour by CQC.
Watchdogs should be protectors, but history shows that they can in fact become bottlenecks.[9]
What would Lord Sugar say to Nero? “You’re fired”?
If Secretary of State, you aspire to “More Gandhi, less Stalin”, please note that Mahatma Gandhi once said:
“Action expresses priorities”.
Please re-align CQC strategy urgently, and please ensure that whistleblowers and would be whistleblowers are not harmed or deterred by any hostile acts of commission or omission.
The safety of patients depends on staff who are free and safe to speak up.
[1]http://www.cqc.org.uk/sites/default/files/documents/cm_0114310_item_10_appendix_1_cqc_framework_agreement.pdf
[2] http://www.theguardian.com/society/2014/nov/22/there-were-hundreds-of-us-crying-out-for-help-afterlife-of-whistleblower
[3] https://sharmilachowdhury.com/2014/12/21/the-nhs-is-allowing-babies-to-be-maimed/
[4] http://www.independent.co.uk/news/uk/home-news/shocking-footage-shows-elderly-residents-being-taunted-and-abused-at-essex-care-home-9303888.html
http://www.bbc.co.uk/news/uk-27906730
http://www.theguardian.com/uk-news/2014/dec/14/labour-pledges-yarls-wood-centre-investigation
[5] https://www.whatdotheyknow.com/request/whistleblowing_nhs_analysis
[6] http://www.cqc.org.uk/sites/default/files/20141208_complaints_matter_report.pdf
[7] http://qualitysafety.bmj.com/content/early/2013/08/28/bmjqs-2013-001947.full.pdf
[8]https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/379803/Christie_Review.pdf
[9] http://www.washingtonpost.com/politics/federal-diary-whistleblowers-get-a-defender/2011/10/18/gIQAtnvfvL_story.html
Care home boss suspended after naming whistleblower
A care home boss who revealed the identity of a whistleblower has been banned from nursing for six months.
Jennifer Kirk was not present at the Nursing and Midwifery Council (NMC) conduct and competence committee hearing but had admitted multiple charges of misconduct.
Mrs Kirk, who was employed as manager at Ashlea care home in Callander, failed to investigate properly an allegation that the deputy manager had been accessing pornographic websites at work.
Concerns had been raised by another employee, named only as Miss 1, on February 1 2013 and Mrs Kirk later told the subject of the complaint who had made it.
In addition, she did not notify the appropriate protection agencies of the incident, and she did not suspend the deputy manager until April 6 last year.
In a written submission to the NMC, Miss 1 stated that she used the home’s computer on January 31 last year and noticed that the internet history showed various pornographic websites had been accessed on January 16.
She took a photograph of the computer screen with her mobile telephone and reviewed the nursing rota, which indicated that the home’s deputy manager was the nurse on duty at the time.
She said she told Mrs Kirk the following day but the manager did not take the complaint seriously.
The deputy manager then made it clear to Miss 1 that he knew she had found the information on the computer and had told Mrs Kirk.
The matter was later reported to the Care Inspectorate in Scotland and Stirling Adult Support and Protection by another member of staff.
The Care Inspectorate ruled that Mrs Kirk should have investigated the concerns properly and protected the identity of the member of staff who raised the complaint.
An internal investigation by the company which runs Ashlea, Mauricare Dumpark Limited, found that Mrs Kirk had breached its whistleblowing policy.
She also admitted making more than a dozen medication blunders in April and May 2013.
She failed to ensure that medication — including anti-psychotic, osteoporosis, painkilling and antibiotic drugs — was administered as prescribed, or recorded as administered, to 10 residents at the home.
Additionally, between April and May 2013 she failed to ensure that there was an effective audit trail of medication received and administered to residents in the home.
Imposing a six-month suspension order, the NMS said: “Given the seriousness of the facts admitted and found proved, the panel considers that Mrs Kirk’s conduct is a serious departure from the standards expected of a registered nurse and, as such, did not uphold the reputation of the profession at the relevant time.
“The panel considered that a period of suspension would be sufficient to protect patients and the public interest.
“The panel noted that Mrs Kirk has had an otherwise unblemished history as a nurse.
“However, the panel has not seen any evidence of remediation and, as such, concluded that Mrs Kirk still represents a risk to patients.”
The NHS is allowing babies to be maimed
Sunday Times 21 December 2014
A PAEDIATRIC surgeon who tried to expose “barbaric and amateurish” circumcision of boys, including babies, is facing disciplinary action for raising his concerns with the patient safety regulator.
Shiban Ahmed has fought for more than a decade to get the Care Quality Commission (CQC) and its predecessor, the Healthcare Commission, to protect children from cheap circumcisions carried out by poorly skilled GPs. In some cases, boys aged six to 10 are tied to tables or forcibly held down while a local anaesthetic is injected directly into the penis. The anaesthetic often proves ineffective and the operation follows with the child still screaming in pain.
Ahmed recently presented a dossier of cases to the CQC. He also accused the regulator of failing in its duty after learning of new examples of “cruel” and unsafe operations in clinics he had previously reported.
The CQC responded by contacting his employer, University Hospitals of North Midlands NHS Trust (UHNM), to allege that he had breached patient confidentiality.
Last week the trust said it was referring him to the General Medical Council (GMC), which has the power to strike him from the medical register.

Ahmed became aware of dangerous circumcisions when he was asked to carry out corrective surgery after botched operations. He believes the only safe place to circumcise school-age boys is in hospital with a trained surgeon.
The cases often involved boys from Muslim families. In most of Britain circumcision for cultural reasons is not available on the NHS and, as the procedure costs at least £1,400 in hospital, parents turn to GPs who charge £200-£300.
Many of the problems were in Birmingham, where the operation is available on the NHS and where the health service pays GPs £190,000 a year to perform circumcisions at a cost of £90 per child.
Some young patients nearly died after circumcisions and Ahmed recalls having to remove part of a boy’s penis. Others lost so much blood they needed intensive care.
The surgeon started touring mosques to publicise the dangers, making clear that he was not opposed to circumcision, which has moderate health benefits, but wished to see it done safely.
He also set up a private clinic to offer circumcision under general anaesthetic at a similar price to GPs. He says he takes no fee from the operations.
As a result of his outreach work, families reported their experiences and he asked consent to pass cases to the CQC.
As some of the case histories were given to him by telephone, Ahmed says he took advice from the information commissioner and the GMC before recording the conversations and passing them to the CQC in a dossier of 22 cases.
“My children were tied down onto the table,” says one of the written statements in his dossier. “My children went through great discomfort through the pain of the operation as well as that of being tied down by heavy strings.”
Another complainant says: “I lost a lot of blood to the point where my life was in danger.”
Two surgery receptionists had earlier told Ahmed how a boy undergoing circumcision ran screaming to a lavatory and locked himself in, bleeding heavily. The child’s father fainted and “pandemonium” broke loose.
“I am still seeing children with the most terrible complications,” Ahmed said. “Some are so bad they cannot be corrected and have left babies and children maimed for life. I cannot understand how the NHS is allowing this.”
Ahmed submitted a file of cases two months ago to Amanda Reynolds, an acting inspection manager at the CQC. They included the recorded telephone calls.
Listening to the recordings, she was uncertain if the correct consents had been obtained and decided to treat them as covert. Reynolds wrote to Ahmed, raising her concerns, but also sent her email to the trust which began looking at the case. However, Ahmed was unable to explain himself to the trust because he had consent from the families to discuss their complaints only with the CQC, not with his employer.
Last Monday, Nick Coleman, the trust’s “responsible officer”, told Ahmed he was forwarding his case to the GMC for investigation.
Ahmed is a serial whistleblower who has made allegations in the past of unsafe surgical practices at Stafford Hospital and at Alder Hey Children’s Hospital in Liverpool.
His concerns at Alder Hey led to an investigation by the Royal College of Surgeons, but the full report has yet to be published. He is suspended by Alder Hey and UHNM for allegedly disclosing patient details to the CQC.
Fiona Bell, an NHS campaigner, called on Jeremy Hunt, the health secretary, to intervene. Hunt has previously said that NHS whistleblowers should be protected.
“I will be writing to Mr Hunt to seek assurances that this brave doctor is not sanctioned in any way for raising concerns to protect children,” she said. “I was told the government supports NHS staff raising concerns so I would expect protection for Mr Ahmed.
“One would expect those who have harmed children to be investigated by the NHS and CQC as well as by the police and social services.”
UHNM said: “Clinicians at the trust are working with the CQC to provide support for one of its non-NHS inquiry’s [sic] following a request for our assistance.”
The CQC denied reporting Ahmed to his trust, even though Reynolds appears to have alerted the trust in her email dated November 4.
“The Care Quality Commission is very concerned about reported cases regarding the safety of circumcisions brought to our attention by Mr Ahmed,” the regulator said. “We listened to these concerns and responded quickly by carrying out a number of inspections at services. We have taken action in relation to what was found during the inspections.
“The CQC has not reported Mr Ahmed to the GMC or to his trust and has not invoked any disciplinary action against him.”
A leading child doctor said that restraining boys for circumcision was illegal and “in the same bracket as female genital mutilation”. Dr Martin Ward Platt of the Royal College of Paediatrics and Child Health said: “It would ride a coach and horses through the rights of the child.”
‘U’ turn from Hunt’s team following media pressure
By Sharmila Chowdhury 14 December 2014
 Fiona Bell, NHS whistleblower and an avid campaigner, wrote to Jeremy Hunt, Secretary of State and Ed Jones, Special Advisor, in 14 October 2014, raising serious concerns on behalf of a Morecambe Bay whistleblower, regarding a nurse who allegedly went around turning off the drips off elderly end of life patients in order to speed up their deaths.
Fiona Bell, NHS whistleblower and an avid campaigner, wrote to Jeremy Hunt, Secretary of State and Ed Jones, Special Advisor, in 14 October 2014, raising serious concerns on behalf of a Morecambe Bay whistleblower, regarding a nurse who allegedly went around turning off the drips off elderly end of life patients in order to speed up their deaths.
Fiona, hoped that due to the serious nature of her complaint, matter would be urgently investigated.
However, to her amazement, Fiona received the following response:
From: <DoNotReply@dh.gsi.gov.uk>
Date: 6 November 2014 16:53
Subject: Response to your Query : – Ref:DE00000892418 – your recent correspondence to Jeremy Hunt and Ed Jones
To: fbell226@gmail.com
Our ref: DE00000892418
Dear Ms Bell,
Thank you for your correspondence of 14 October to Jeremy Hunt and Ed Jones about Mr xxxxxx. I have been asked to reply.
The Department of Health has noted the concerns in your correspondence. However, as mentioned in previous replies to you, ministers and Department of Health officials are not in a position to discuss personal employment issues.
Thank you for raising your concerns.
Yours sincerely,
Jeremy Vooght
Ministerial Correspondence and Public Enquiries
Department of Health
Shockingly, Department of Health instead of urgently investigating, responded by viewing early demise of the elderly patients as an employment issue and refused to comment.
Fiona, in her true form, refused to give up and wrote again:
Clearly, it still takes a determined campaigner, the media and public pressure to direct the Department of Health into appropriate action. This is despite of much publicised NHS whistleblowing cases, and promises of change by the Secretary of State, who commissioned the Francis’s review. We have a very long way to go.
For more details on the case: https://sharmilachowdhury.com/2014/12/14/ignoredwhistleblowers-claim-of-nurse-who-killed-slowly/
‘Landmark legal win’ for cardiologist Dr Kevin Beatt sacked by Croydon Hospital for whistleblowing on patient safety
First published Wednesday 3 December 2014 in Local news
Last updated 14:10 Thursday 4 December 2014
Your Local Guardian: Photograph of the Author Exclusive by Chris Baynes, Reporter
Dr Kevin Beatt was unfairly dismissed for raising concerns about safety at Croydon University Hospital
Dr Kevin Beatt was unfairly dismissed for raising concerns about safety at Croydon University Hospital
A leading heart doctor who blew the whistle on safety following a patient’s death at Croydon University Hospital was unfairly dismissed amid a calculated attempt to damage his reputation, a tribunal has ruled.
Consultant cardiologist Dr Kevin Beatt stands to receive thousands of pounds in compensation following his landmark victory in a two-year legal battle with Croydon Health Services NHS Trust.
The trust sacked him in September 2012 after he raised the alarm about staffing shortages, “appalling” equipment and workplace bullying.
From July 2013: Man dies during routine operation at Croydon University Hospital after lead nurse is suspended
From June 2014: Croydon University Hospital suppressed safety concerns after patient death, claims ‘whistleblower’ Dr Kevin Beatt
Dr Beatt, a renowned specialist who led the hospital’s well-regarded department for interventional heart procedures from 2007, should have been afforded protected whistleblower status.
But instead he lost his job in a case he claimed provided a damning demonstration of the trust’s attempts to cover up failings.
The trust argued it had dismissed him “for making unsubstantiated and unproven allegations of an unsafe service”.
PROMOTED STORIES
The continuing rise of Indian Philanthropy (The Economist on UBS)
Mourinho to recall £150,000-a-week star; Newcastle vs Chelsea predicted line-ups (Give Me Sport)
Conflict Minerals: One Company Actually Doing the Right Thing? (Intel on Mashable)
Christmas posting dates for UK & overseas (Post Office™)
The little island perfect for the fishing trip of a lifetime (High50)
5 Reasons You Should Consider Remortgaging (Experian)
Recommended by
But the employment tribunal ruled there was “no consistent evidence” of misconduct and that chief executive John Goulston, whose evidence it criticised as inconsistent, had “failed to carry out a fair process”.
Mr Goulston was interim chief executive at the time Dr Beatt was sacked after joining from a regional provider development role with NHS London in May 2012. He became chief executive of Croydon Health Services NHS Trust in February 2013.
The London South Employment tribunal ruled the doctor was unfairly dismissed solely or principally because he made a protected disclosure.
It is believed to be the first time an NHS whistleblower has won such a legal dispute on that point.
Between 2008 and his dismissal, Dr Beatt raised a catologue of concerns about inadequate equipment, bullying and harassment of junior employees, removal of key staff, a lack of competent nurses and the failure to properly investigate serious incidents.
In January 2010, he voiced serious fears to then medical director Tony Newman-Sanders that the cardiology unit’s radiation equipment, the oldest in use in the country, was putting patients and staff at risk.
He was accused of fabricating his concerns so he could treat patients elsewhere, but six months later the machinery was condemned and replaced after breaking down during an operation.
Friction between the cardiologist and hospital directors came to a head in July the next year, when a 63-year-old patient died during a routine procedure after a senior nurse was suspended without Dr Beatt’s knowledge.
Dr Beatt, who was left for 20 minutes without a nurse with even basic familiarity with the operation, described the suspension as “the most overtly reckless act” he had witnessed in his career.
He said he would not have begun the procedure had he known the nurse had been suspended.
The tribunal heard that four days after the death Dr Beatt was verbally threatened by Nick Hulme, then the trust’s chief executive.
Mr Hulme, who resigned in February 2012, allegedly warned the doctor not to make accusations about his managers in relation to what happened.
Mr Beatt told the tribunal: “I felt very intimidated by Mr Hulme’s statement and it was a clear warning to me that the trust did not want me to raise patient safety concerns and wanted to protect the management team from any suggestion that their decision to suspend Sister Jones may have contributed to the death.”
Your Local Guardian:
‘Intimidation’: Nick Hulme, the trusts’s former chief executive, allegedly threatened Dr Beatt
The trust claimed Dr Beatt’s criticisms were “vexatious” and calculated to ensure the restoration of Sister Lucy Jones, and in September 2011 it began disciplinary proceedings that culminated in his sacking.
But at an inquest at South London Coroner’s Court last year, coroner Dr Roy Palmer ruled Sister Jones’s absence had contributed to Gerald Storey’s death.
And the tribunal found there was “no evidence” Dr Beatt had an ulterior motive and that “extremely damaging” and “entirely false” allegations had levelled at him during a investigation into the Mr Storey’s death.
Those included claims by Dr Asif Qasim, the hospital’s clinical lead for medical specialities who had been repeatedly accused of bullying staff, that Mr Beatt was mentally unstable.
Witness statements made to the serious untoward incident inquiry into Mr Storey’s death had also been altered, the tribunal found.
Employment judge Gill Sage, the tribunal’s chair, said: “The tribunal therefore conclude on all the evidence before us that the respondent has not shown that the reason for dismissal was misconduct.”
She added the panel believed a “misleading” press statement about Mr Beatt’s dismissal, issued following the inquest 10 months later, had been “calculated and was likely to cause damage to his reputation”.
The tribunal, which sat between May and October this year, also unamimously ruled Dr Beatt had been subjected to detriment as a result of making a protected disclosure as a whistleblower.
But it dismissed a claim for unauthorised deduction of wages because Dr Beatt had not raised a grievance within the designated time limit.
Your Local Guardian:
‘Inconsistent’: Chief executive John Goulston’s evidence to the tribunal was criticised by the judge
After tribunal’s ruling, Dr Beatt told the Croydon Guardian he believed the trust systematically tried to silence concerns.
He said: “Essentially they ignored some of the statements made to the serious untoward incident report and submitted their own version.
“There’s no doubt in my mind that what they do is, if things have gone badly wrong, instead of saying things have gone badly wrong, they try to cover it up.
“The bigger picture here is it’s not just this case they’ve done it on. They’ve done it on lots of others.
“At the end of the day it is in order to misrepresent events to the patient and their relatives. That needs to be exposed.”
He said the legal battle and the trust’s decision to refer him to General Medical Council had taken “a very considerable toll” on him and left him unable to find work within the NHS, adding: “That’s why they do it.
“They do it because it will prevent me from getting a job and that will prevent me from pursuing them in court because I won’t be able to afford the costs.”
Dr Beatt said he believed the trust had spent “more than £100,000” fighting his case, which he was only able to pursue because his lawyers Linklaters agreed to work pro bono.
A spokesman for Croydon Health Services NHS Trust said it would appeal the ruling.
He said: “We are clearly very disappointed with the tribunal’s decision.
“Having sought legal advice, the trust is in the process of submitting an appeal against the judgment, to the Employment Appeal Tribunal.
“We take all concerns about patient safety extremely seriously, as well as allegations of bullying against any of our employees.
“It is everyone’s responsibility at Croydon Hospital Services to uphold great care for patients, and for our staff to know that they will be listened to and supported.”
Jeremy hunt: Message to NHS Staff on transparent, safe healthcare
The Secretary of State for Health talks about new regulations for a more open and accountable healthcare system and the launch of MyNHS.
As part of our determination to make the NHS the safest and most transparent healthcare system in the world, I want to tell you about two new important regulations that came into force yesterday.
The first is the Statutory Duty of Candour, which places a legal duty on hospital, community and mental health trusts to inform patients of mistakes which have led to significant harm or death. This is a key response to Francis, and a significant step towards a more transparent and open NHS. At the same time, the General Medical Council and Nursing and Midwifery Council are consulting on a new Professional Duty of Candour which would mean that there would be an obligation on doctors, nurses and other health professionals to inform patients when something goes wrong. This is all designed to bring concerns into the open much more quickly, so that we develop a learning and improvement culture. I hope it will mean the NHS becomes the first healthcare system in the world that starts to get close to eliminating avoidable harm, including the 1,000 avoidable deaths we have every month across the system.Jre
The second new power is about ensuring strong and safe leadership in healthcare organisations. Under new regulations, all NHS board members will be required to undergo a Fit and Proper Person’s Test before they are appointed. During its inspections, the Care Quality Commission will check that NHS Trusts have strong systems in place to ensure they are appointing the right people to hold these important roles. Importantly, the Care Quality Commission now have the power to remove directors who have overseen poor care. These tests will be extended to care homes in April 2015.
Finally another step towards creating a more transparent and accountable culture was the formal launch of MyNHS last week, a new part of the NHS Choices website that enables patients and professionals to compare the performance of hospitals, consultant services, GP practices, care services and local authority. MyNHS includes searchable data on staffing, patient safety, mental health and food quality, along with many other areas of care. Over time, more data will be added and MyNHS will become an increasingly powerful resource for patients, doctors and local NHS commissioners.
We should be proud that we are probably already the most transparent healthcare system in the world – this will take us even further. So thank you for the part you are playing to make it possible.
‘There were hundreds of us crying for help’: the afterlife of the whistleblower
Whistleblowers speak out because they feel they have to, often at great personal cost. But years later, do they think it was worth it?
 Andrew Smith The Guardian, Saturday 22 November 2014
Andrew Smith The Guardian, Saturday 22 November 2014

In his former life, Dr Raj Mattu was an internationally recognised cardiologist. On course for a professorship in London, he nonetheless jumped at the chance to return to his home town of Coventry in 1997, to set up a medical school at Warwick University and help turn the large district Walsgrave hospital into a teaching facility. It was a choice he would live to regret.
He found problems straight away. Patient safety was at risk through broken equipment and misallocation of resources; there were factions among staff and tensions with management. In the months before he arrived, senior clinicians had narrowly failed to pass a vote of no confidence in CEO David Loughton. Little was as it should be.
As the youngest consultant but one of the best-trained, Mattu worked long hours trying to improve things. All the same, one issue kept returning: the so-called “5 in 4” system of squeezing an extra bed into cardiac wards designed for four, a policy that left essential services such as oxygen, mains electricity and suction less accessible to some patients. Already convinced this was quietly costing lives, staff including Mattu pleaded for the practice to end, but management wouldn’t listen.
When the inevitable day came, it was on Mattu’s watch. A man of 35 went into cardiac arrest and staff could neither reach the tools they needed nor rearrange the beds in time. They watched in shock as their patient’s life drained away; afterwards the furious cardiologist and two senior nurses filed a serious clinical incident report. The 5-in-4 policy was not reviewed.
Now cardiac consultants passed a vote to replace their management-friendly clinical director with Mattu, but CEO Loughton rejected their choice. Instead, Mattu was offered a pay rise, which the medic interpreted as trying to buy his silence, and refused. When the Care Quality Commission (CQC) came calling in April 2001, he was one of five clinical staff to raise the alarm. Mystifyingly, the CQC passed the complainants’ names to Loughton. Yet when its report emerged that September, chief executive Peter Homa spoke of the “worst ever [patient safety report] produced for any Trust” and an “excess death rate” of 60% (against a subsequent high of 29% at the notorious Mid Staffs).
When Loughton denounced the CQC findings, and insisted to the BBC that no one had died or been harmed because of the 5-in-4 policy, something snapped inside Mattu. After taking advice from the General Medical Council (GMC), British Medical Association and Medical Protection Society, Mattu appeared on Radio 4’s Today, revealing that, in the opinion of medical staff, at least two patients had died unnecessarily on overcrowded wards, and that management knew and had done nothing. So a whistleblower is made.
***
Whistleblowers have always been with us, but this century they have attained a kind of ubiquity, leading the news on a weekly basis. Last month, a whistleblower reported massive accounting irregularities at Tesco; this month it was alleged mortgage fraud on an unimaginable scale at JP Morgan Chase. As I write, allegedly dangerously lax hygiene at a dental practice in Nottingham has been revealed. And all this whileLaura Poitras’s documentary about Edward Snowden screens at cinemas around the country.
So why now? Partly, it’s because economic self-interest has become king. If a senior executive earns £400k, or £1m, he or she has a lot to lose. A whistleblower is a threat to the business – and in UK law, a threat to a management whose first legal duty is to shareholders, rather than customers or workers. Globalisation and the internet have further loosened the old social and commercial ties.
Who are the whistleblowers, and what makes them do it when most of us don’t? The Hollywood-created image is of the awkward outsider; brave, but destined for maverick isolation anyway. In short, not like us. But most of the people I meet in the course of writing this article are essentially conservative. They spoke out because they felt they had to. The real story lies in what happened next.
***
Last month I sat in Raj Mattu’s kitchen, eating biscuits and drinking tea. He told me that the decision he made back in September 2001 still haunts him every day, that his lives then and now might as well belong to different people.
At medical school, he had trained with world-renowned experts, been drawn to cardiology, and risen through the ranks fast. Then came Coventry. After Mattu spoke to the BBC, management moved quickly, and a disgruntled temporary doctor levelled a charge of bullying against him. Mattu and two fellow consultants were suspended; all were prevented from talking to colleagues or the media, their disputes recast as employment matters rather than public interest disclosures.

Soon, the single complaint against Mattu had become 35, then 200, ranging from questions over his qualifications to charges of serious criminal conduct outside of work. These were sent to the GMC, CQC, the Strategic Health Authority and three different police forces; by 2009, all had been investigated and found to be false. Mattu was also subject to three separate tax inquiries, despite having undertaken no private work. In 2010, ill and suffering from depression, he was finally sacked by managers who questioned the validity of his ailments and found him “unmanageable”.
Before we met, Mattu and I spoke several times on the phone, including one conversation so full of names, dates and surreal events that I almost doubted his sanity. Two hundred charges? How could there be that much smoke without a fire? He sighed. “You clearly come from the same world I like to live in. But what you describe is not what happens. I’m not alone: there are hundreds of whistleblowers crying out for help. In fact, I’m almost unique in that I’ve come out the other end.”
Last April, 13 years after Mattu spoke up, an employment tribunal that ran for six months produced a remarkable 400-page document that detailed the systematic destruction of one man’s career by managers, some of whom remain in the NHS and one of whom, David Loughton, isnow a CBE. The report found that management had created a culture of fear, and Mattu had been victimised for raising concerns over patient safety; he will be awarded compensation. The case against him, meanwhile, is thought to have cost the NHS £6m-£10m so far.
Today Mattu betrays little bitterness, and says he was helped by a city-wide campaign. Local ska band the Selecter played a benefit and at a celebration party, attended by 1,200 people, where singer Pauline Black(a radiologist) duetted with him on the Beatles’ Let It Be and Hey Jude. Music, he thinks, has kept him sane. Two years ago, his wife Sangeeta secretly entered him for the Voice; he was invited to the heats, but didn’t find the time to go.
But there were dark times, too. The couple had wanted to start a family, but felt unable to while the case was ongoing. Now they are thinking about it. And you know what? Theirs is the happy story.
***
Eileen Chubb’s story reads like a lost chapter from One Flew Over The Cuckoo’s Nest. Sitting in her south London garden, it occurs to me that her apparent ordinariness is what makes her so remarkable. She provides a window into the mechanism of whistleblowing, and also our curious, contradictory response to those who do it.
Chubb left school at 16 and worked as a manager in a local bakery chain, before deciding on a career switch in her early 40s, following her mother into care. With no experience, she opened the phone book and called the first care home she saw. Isard House was run by Bupa for Bromley council, and she was offered a job at once, on the advanced dementia unit. “It’s hard work,” she says, “but caring for those people was a privilege, because they were special, priceless. The trick was finding a way through to them. And there always was a way.”
Chubb talks about the residents she loved: Lil, a mischievous Scot in her mid-90s with a penchant for cutlery hiding and late-night booze-and-chip expeditions. And Jessie, who could scarcely speak and was afraid of the bath, until Eileen discovered that if she sang Daisy, the fear would vanish and words would come back as she sang along.
Chubb’s appointment as team leader to another unit was bittersweet, because she had enjoyed her own and respected the staff. But when she returned to check on her friends, she found something had gone terribly awry. A new team leader seemed to spend most of her time watching television, while residents slept in their own urine and went unfed. Several times, Chubb found her shouting or pushing residents, with junior carers following suit.

Chubb raised her concerns; nothing happened. Finally, after hearing that six colleagues had done the same, she wrote to Bromley social services. Fearing a backlash, she offered the other six the chance to lie low, but they all stood by her as the horrified head of social services launched an investigation and informed police, who raided the home and made arrests. A subsequent report found painkillers had been withheld, unprescribed drugs dispensed on a whim and records falsified.
Game over? No. Bupa attacked the report; a campaign of intimidation by care home staff began, and two of the group were forced off sick with stress. A year later, an industrial tribunal found in the seven’s favour, its report a study in establishment fudge. It was later revealed that there had been no prosecutions because there had been no police investigation; the problem staff, including the team leader, had been dispersed to other Bupa homes.
Led by Chubb, the Bupa 7 refused to accept the tribunal’s ruling or any compensation payment, and rejected substantial payoffs the company offered in exchange for silence. After two years of fighting and being unable to get work in the care industry, most were in dire financial straits, despite huge public support: at one point, the local paper gave them jobs as cleaners. Undeterred, Chubb bought the Penguin Guide To Law, for £3.99, and set out to hold Bupa to account.
That was 13 years ago. Two of the seven are working in care again; the rest have rebuilt their lives around other things. Chubb runs a charity, called Compassion in Care, and is a founder of the Whistler, which fights to expose poor conditions in care homes and to help those who speak out. A powerhouse of citizen activism, she is driven not by ideology but by a simple sense of right and wrong. She dates her transformation to her first meeting with Bromley social services, when she opened her mouth to speak and was startled by the voice that emerged – clear and ice-cold with rage.
“People who didn’t know me then never believe this,” she laughs, “but I was the sort of person who didn’t make a fuss. I had a soft voice and if I had to say something, I’d say it nicely and quietly.”
There was no history of rebellion, not even at school? “Oh no, I wouldn’t get my socks dirty. I was scared of my own shadow. But those people in Isard House were easy to fight for. Someone like Jessie should have been cared for in her old age, not dragged down a corridor screaming.”
She was never tempted to take the money? “Not if they’d offered a million pounds. If the judge had awarded us money and condemned Bupa, fine, but taking the money with no admission of guilt would have been insulting all those who’d been abused. If Bupa didn’t accept responsibility, then other people in other homes would pay the price. To allow them to cover it up by paying us would have made us abusers as well.” Almost as an aside, Chubb recalls her father, a construction worker, being so deeply affected by the death of a young co-worker who drilled through a mains cable that he organised a whip-round for the family, and remonstrated so forcefully with site managers that he was out of work for some time afterwards.
She admits her new life has cost her friends, mostly because her politicised interest in the world leaves her easily bored by everyday, trivial concerns. In any case, campaigning is her life now and money is still tight. As with Raj Mattu, the most curious thing is the way former colleagues, those who had been guilty of no wrongdoing, turned on Chubb and her small cohort after they raised the alarm. I could see no sense in this behaviour, but it turned out to be key.
***
C Fred Alford, professor of government at the University of Maryland, is the author of Whistleblowers: Broken Lives And Organizational Power, a study into the personal impact of whistleblowing. It makes for an alarming read. Surprise discoveries include a finding that seniority offers little protection, and that it makes no difference whether a concern is first raised inside or outside the organisation. Of Alford’s three dozen-strong sample group, most lost their jobs and never worked in the same field again; many also lost their families, as court cases and tribunals dragged on for a decade and more. A majority suffered from depression, with alcoholism common. In another study, half the sample group was found to have gone bankrupt. All of this tallied with the people I talked to: the sanctity of whistleblowing may be written into law, in both the UK and US, but for most it will be a traumatic experience. “The greatest shock,” Alford says, “is what the whistleblower learns about the world – that nothing he or she believed is true.” Hence the “nuts and sluts” narrative we find in relation even to celebrated whistleblowers such as Karen Silkwood, Erin Brockovich, Julian Assange and Edward Snowden. This is a narrative we embrace, because it makes us feel secure: they brought it on themselves.
***
A common cry after the financial crisis of 2008-9 was, “Why did nobody see this coming?” – but the best risk management execs had. In the US,Eileen Foster, executive vice president of fraud risk management at the giant Countrywide home loans company, saw and called the mortgage irregularities that earned CEO Angelo Mozilo a staggering $470m between 2001 and 2006 (the vanity plate on his car read FUND-EM) and would play an outsize part in sinking the US economy. She was proved spectacularly right, but claims to have had 145 job applications turned down thereafter. Her colleague Michael Winston, a board member, was similarly dumped and pilloried after refusing to write a report for Moody’s credit ratings agency that he believed would be false.
Paul Moore was head of risk management at HBOS, a holding company for the Royal Bank of Scotland and Halifax brands. HBOS gambled on bad mortgages and payment protection insurance (PPI) and lost £10bn in 2008. It was bought by Lloyds, then rescued with £37bn of public money. HBOS did more than any other institution to bring UK banking to its knees – but it had been warned.
Moore trained as a barrister and went to work for a financial services firm in Swindon because he knew the hang-gliding would be good. From there he moved through American Express and KPMG before joining HBOS in 2002. Asked whether his job involves annoying managers, he admits that willingness to deliver unwelcome truths is important, but adds, “Risk management is not about going slowly, it’s about going as fast as you can and managing the risk. Formula One has less residual risk than angling, for instance. So I’m the risk management adviser, and the chief executive is the driver. It’s my job to say, ‘Hang on – if you carry on that way you’ll blow up the engine, or run out of fuel, or make the brakes too hot.’”
Has he often been placed in that position?
“I’ve seldom said, ‘You’re going to blow the engine up!’ But I did at HBOS.”
Alarm bells rang in late 2003, when he noticed 12% of profits were coming from the sale of mortgage PPI. He looked across the business and saw aggressive managers pressuring staff to meet wild sales targets (“We’ll never hit our sales targets selling ethically,” one told him), and non-executive directors with insufficient expertise to apply oversight. Worse, upon asking questions, he found “a cultural disposition to resist challenge, often aggressively”. Regulators were worried, too: if their insistence on raising the amount of cash HBOS had to keep in reserve had been made public, as it should have been, negative market reaction might have forced a rethink. But HBOS’s CEO, James Crosby, was also a non-executive director of the main regulatory body, the Financial Services Authority (FSA).

When HBOS paid its auditors KPMG $1.2m to investigate Moore’s claims, its report questioned not just his views, but his professionalism, integrity and stability. Already sacked by Crosby and shunned by former colleagues, Moore says he read the report and wept. “The auditors and accountants are at the rotten heart of everything,” he says. “You know, I got to the point where I actually thought they were right and I was wrong. I came to think I must be a terrible person.”
In contrast to Eileen Chubb and the Bupa 7 – and more typically of whistleblowers – Moore was on his own. For the first time in his life, he began to sweat to the point where he had to wear sanitary towels under his arms in meetings and – already a heavy drinker – he grew capable of downing a bottle of vodka in half an hour, terrifying his wife and confusing his children. He reads me a birthday card from his then 17-year-old son: “Everyone has flaws,” it says. “I like to look past the flaws and see the good in people, and there’s a lot more good in you than you give yourself credit for. I truly am proud of you and everything that you stand for, which is mainly integrity and truth. Just stay true to yourself and keep on doing what you’re doing. It’ll all work out eventually.”
Fired 10 years ago, Moore says he has gone into recovery only this year. “When I say it nearly killed me, it’s not a metaphor. I am a confident, resilient person. To crush me is a serious thing.”
Moore sued HBOS for unfair dismissal and accepted a half-million-pound settlement – in return for his silence. It was to presage the worst of his crisis: “I remember lying on my bed, seeing duty to my family on the one hand and knowing these people have got away with blue murder on the other. You’ve sold your soul to the devil.”
Later I am contacted by another casualty of the banking industry, a financial adviser in a branch who saw mis-selling by policy, reported it and was turned upon by company and colleagues. Like Moore, Lynne Edwards accepted a payoff and signed a gagging clause four years ago, encouraged by lawyers eager to be paid. Like him, she’s haunted by it. “If I knew then what I know now, about how it eats away at you and keeps going on… The bank paid their fine and carried on as before. When I go to job interviews, they ask why I left and I have to lie, so I’m still in limbo. What’s it been for?”
Perhaps most shocking is her contention that her former employers lied to regulators. On reading the FSA’s report, she tried to warn them. “But they said, the bank has been fined now, so it’s dealt with. I was referred to the whistleblowers’ helpline. It ends up being a burden: you’ve done it, you’ve blown the whistle, and that’s what you are from that point on. You’re a whistleblower.”
Kate Kenny of Queen’s University in Belfast and Harvard’s Safra Centre, author of a book about whistleblowing in the finance industry, says she has been surprised by “the amount of work that goes into a being a whistleblower”, meaning the constant reading of documents, rebutting of arguments, exposing of lies and learning about the law, all while struggling to hold your personality together: in short, by the fact that it’s a full-time job which – usually without warning – takes over your life.
Of my sense that whistleblowing is on the rise, she says: “In finance it’s too early to tell. The regulators are receiving more tipoffs, and yet no whistleblower came forward about Libor.”
***
Why is the psychological impact of whistleblowing so extreme? David Morgan is a psychoanalyst who works with whistleblowers, often on a pro bono basis for clients who have lost their livelihoods. “At first, when they talked about how paranoid they were and how many people were after them, I saw them very much like ordinary patients and treated them accordingly,” he says. “But after two or three months I became paranoid myself: I realised what they were talking about was real, not just a mental health issue – their lives were under threat.”
Is there a process of recovery, as with alcoholism or bereavement? “Yes, there are three stages. First, ‘I’m gonna do it’ and the excitement about standing up and being counted. Then there is disillusionment, when you realise you’ve been left standing on your own and that colleagues who said they’d stand by you haven’t. And the third stage is that any underlying psychological problem, to do with a relationship, depression or whatever, is exacerbated enormously. There’s a real feeling at this stage that they’ve lost everything.”
The therapist’s job is to help a patient find something good in their life to hang on to. Most of us like to think we would stand up and be counted when faced with wrongdoing, but the hard truth is that most of us don’t. What makes whistleblowers different? Most of us, Morgan suggests, employ psychological mechanisms such as “splitting” to manage moral conflict (in other words, we don’t think about it too much); whistleblowers don’t. This means those most inclined to do it are the least equipped to cope psychologically. They often also have a courage drawn from an ideology, religion or strong set of principles, Morgan adds, from “a sense of belonging to something greater than the organisation they work for, whether God, humanity or some broader community”.
Are there any who don’t recover? “I’ve seen people go mad, yes, and start to identify with their attackers or turn in upon themselves. It’s very frightening. People are suddenly plunged into a world they didn’t know existed, where the rules they thought applied don’t. Think about it: you do something idealistic, because you think it’s right, then you end up being seen as the corrupt one. And one can always find some reason for blaming oneself, at which point people can really struggle. Someone like Eileen Chubb, who has this huge ideological underpinning, this belief in care and compassion, is at a real advantage.”
Chubb also had a group around her and a supportive husband. What if you don’t have that? And what if you have an entire nation ranged against you? Christoph Meili is Swiss, and was working as a security guard when, on his rounds one night, he stumbled across a tranche of second world war era records in a storage room at a major insurance company. Interested in history, he looked more closely and found ledgers full of insurance policies held by German-Jewish customers up to 1945, at which point they were unilaterally frozen by the company. Of special poignancy were stacks of letters from destitute Holocaust survivors and victims’ families, begging for the policies’ terms to be met – all dismissed on spurious technical grounds. Security is a respected occupation in Switzerland and Meili could boast two degrees, but he didn’t need them to recognise these papers as significant, so he hid a handful in his coat and found a photocopier, but in the time it took the machine to warm up, he lost his nerve.
Two weeks later, he found another large stash of historical documents at the giant bank UBS, including two black ledgers detailing loans made to German companies before and during the war. Among these companies were a maker of chemicals used in concentration camps and others active at Auschwitz. As the war neared an end, corporate registrations had been transferred to Swiss banks in order to keep their assets from the Allies.

But there was worse, because Meili realised this was no archive store: it was a shredding room. He looked closer and found details of profit accrued from the “forced sale” of real estate in Berlin between 1930 and 1945 – knowledge of which banks had always denied. He knew that the Swiss government had just passed a law forbidding destruction of war records, but also that – technically at least – to take them would be theft.
He took the ledgers home, parked them on his kitchen table and went out to walk the dog. A voice in his head said, “It’s not your responsibility, this is serious, take them back” but another voice wouldn’t let him. His worried wife suggested handing the files to a Jewish cultural group she knew. So Meili did, expecting that to be that.
Two days later, a Jewish community leader pulled up in a big black Mercedes, with news that the UBS papers had been passed to financial police in Zurich. Meili was speechless. Scared. “You’re a smart guy – you’ll be OK,” the man said, but the next day Meili arrived home to find a lawyer there, inviting him downtown to make a statement, just as news arrived that he had been suspended from work. He took his wife and children (whom he’d had to scold for scribbling on the ledgers) for a burger, then stepped into a bizarre new future.
A press conference was called. Meili told reporters the information he had released belonged not just to the Jewish community, but to the public at large: “The Swiss people should know their banks were involved with Nazi corporations.” Now the world’s press was on his doorstep but, as nearly all whistleblowers will tell you, he found this comforting, because the press lent protection and support. For three weeks, Meili was a hero and the banks promised to set up a $200m fund for Holocaust victims. He met some elderly survivors who would now be helped, and he felt good. But the feeling didn’t last long.
Meili’s problems started when the US-based Anti-Defamation League arrived to present him with an award and announce the creation of a $36,000 legal defence fund in his name, while also launching a $28bn lawsuit on behalf of Holocaust victims against the banks. “The problem is that what I did wasn’t about money,” he says. “It was about history and helping the poor people whose lives had been ruined by what these banks had done. But when money came into the picture, so did politics.”
Now the Swiss public assumed him to be rich (he was unemployed and on benefits), and the mood changed, emboldening an already cagey indigenous media to weigh in with stories painting him a liar and a traitor; a turncoat who couldn’t follow orders; a gold-digger and even a Mossad agent. Then the Swiss authorities launched a judicial investigation intohim.
As with Chubb and Moore, the rightness of Meili’s actions is so clear that the narrative of his life from this point on is hard to credit. Following death threats to him and his family, an Act of Congress signed by the then president Bill Clinton granted them shelter in the US on 1 January 1997. The US Jewish community organised a stipend to help while framing a case against the banks. Meili claims to have been handed 35 humanitarian awards in the years after he blew the whistle, but still he struggled to find work. His wife left with their children; he later remarried and had another child, but struggled to support that family and, rootless, lost them, too.
Five years ago, Meili’s mother persuaded him to return to Switzerland and he sits in his small living room in Wil, near Zurich, as we Skype. When he arrived home, the Swiss Broadcasting Corporation website ran a piece headed “Christoph Meili returns – as hero or villain?” which looks bizarre from all but a banker’s perspective. He has been on three different work programmes since returning and attended a mental health clinic, “because I needed some help, you know, my self-esteem was so down, I had to build myself up again.” He says his eldest daughter, now 21 and studying at an American college, has just been to visit, but that her brother won’t speak to him. He works part-time selling Bosch tools, and a third marriage has been good so far, which is perhaps why he’s able to laugh again. “But it’s not the same. I miss my kids. I’ve missed them growing up, it was taken from me.”
He has an outstanding lawsuit against a Swiss newspaper, he tells me, because every two years a tabloid returns to harass him. So he’s still a pariah? Now he softens. “Actually, it’s getting better. Every Saturday at work I have one or two people look at me and go, ‘Hey, you’re that guy!’ but most are nice about it now. After the financial crisis, they say, ‘You’re the guy that first came out against these banks.’ And then they’re happy to see me.”
Which is all to the good, but still some way short of a happy ending.
***
Why do we idealise whistleblowers in the abstract, yet turn on them so readily in the flesh? The loneliness and isolation that comes with the territory seems to feed our view of them as weird misfits who have merely found their natural state. In the words of one, quoted by Professor Alford in Whistleblowers, “I have seen the truth and the truth has made me odd.” That perception is self-sustaining. Why do we need it?
In search of an explanation, I wind up at the door of 81-year-old Dr Philip Zimbardo, conductor of the 1971 Stanford prison experiment, and latterly called as an expert witness to the Abu Ghraib trials. His experiment has been repeated countless times around the globe, with a multitude of variables, and is soon to be revisited in a Hollywood movie starring Billy Crudup.

Famously, Zimbardo’s study involved dividing a group of students into prisoners and guards, then monitoring their behaviour. But within six days the proceedings had to be stopped, as guards grew brutal and prisoners passive and distressed. Most surprising was the apparent fact that personality type (as tested beforehand) afforded little indication of how particular individuals would act; that the most important predictive factor was situation. In conjunction with his former classmate Stanley Milgram’s eponymous and equally groundbreaking experiment, in which test subjects were persuaded by authority figures to administer apparently painful – even fatal – electric shocks to people they believed also to be test subjects, Zimbardo’s research is compelling. Stir in fellow psychologist Solomon Asch’s finding that even the strongest-willed individuals find the burden of standing out from the crowd unbearable over time (in this case a classroom full of peers briefed to answer questions wrongly) and we have a clear picture of ourselves as social creatures who, for the most part, would rather be wrong than isolated.
What does this mean? That our healthy and necessary desire to be social can be turned against us within bad systems, or by bad leaders. Or, as Zimbardo says, “The potential for perversion is inherent in the complexity of the human mind.” Further, where our desire to be social clashes with our underlying values, “we will go to remarkable lengths to bring discrepant beliefs into some kind of functional coherence”. Which is to say, we protect ourselves by rationalising. This is precisely what the whistleblower doesn’t do.
Zimbardo has just launched an organisation called the Heroic Imagination Project, which aims to furnish people with the psychological skills they need to become whistleblowers. “Stanley [Milgram] and I were interested in the same question: how do ordinary, normal people get caught up in these awful things that keep happening, from the Holocaust to Rwanda. And part of the answer is to look at people who don’t, and find out what we can learn from them. For me, whistleblowers are people who are simply more attuned to a situation, who are able to step back, even where they’ve been closely involved in things, and go, ‘Oh my God, this is wrong. How can I stand up or speak out to try to change it?’”
Encouragingly, he thinks this can be taught. “With the project, we’re trying to train ordinary people to be willing to do the right thing. So we’re running programmes, mostly focusing on high school and college students, because we can train them in basic psychological principles that encourage them to speak out – but to take wise and effective action, not risky, not dangerous.”
Asked for a single piece of advice, he offers: “Ideally, whistleblowers should always form a small team, because when you’re a whistleblower against a powerful system, the system dismisses you as a fanatic. But if you have three people, what you’re saying becomes a point of view.”
No wonder professor Alford says that “everything you need to know about whistleblowing, you learned in kindergarten”. Perversely, he goes on to claim that this is a greater problem in individualistic western cultures than in societies where conformity is overtly valued. “Research shows that in Korea, say, they know how groupish they are,” he says. “What happens in America – you know, the land of the free and home of the brave, where the lone sheriff rides in and cleans up the town – is that we have this language of independence and we don’t have a language to talk about how utterly cowardly we are when faced with group pressure. We’re all afraid of stepping out of line. And whistleblowers don’t like it, either, which is why support groups are so terribly important.”
The good news is that whistleblower support and advocacy groups are springing up everywhere, in the UK and abroad. While writing this, I received daily updates from whistleblowingtoday.org. In the UK,compassionincare.com, thewhistler.org, whistleblower.co.uk andWhistleblowers UK all offer support to anyone courageous enough to need it. And while the UK’s ineffective public information disclosure legislation has been sunk further by the government’s introduction of £2,000-plus charges to access employment tribunals (leading to a 70% drop in the number of claims), US legislation is producing results.
Louis Clark of the Government Accountability Project (Gap) in the US, which champions public and private sector whistleblowers, describes his organisation’s tactics as being about replacing the lost “circle of support” with a new one, drawing on those who might benefit from the released information. As the aggressor agency tries to focus attention on the whistleblower, Gap turns the attention back to the original problem. At this stage, Clark tells me, it’s amazing how often relationships within the aggressor group start to break down.
Better still, US law recognises whistleblowing as positive: once a worker has been accepted into this category, sacking them becomes extremely difficult, requiring the production of “clear and convincing evidence” that it would have happened anyway. Just as importantly, the Department of Justice can and does insist that a worker be given their job back pending any court case or tribunal.
“I think whistleblowing is happening more because people believe it can make a difference,” Clark says. “These days we seldom lose a case when there’s a public hearing. And it was noticeable that the argument about Edward Snowden in the US was not over whether whistleblowing is good – it was about whether he counts as a real whistleblower. That’s a big change and in time it will change us all.”
Personal issue or does this need of further investigation? You decide
Whistleblowing in the NHS – how safe are you?
This is a question for staff and patients in the NHS.

Sharmila Chowdhury 4 August 2014
As an NHS staff if I suspect something is wrong, simplest thing would be to raise my concerns to my line manager. Simple. After all, we have decided to work for the NHS because we care? We care for patients and other staff who are placed under our care. Our managers would be grateful to us, surely, and make arrangements to investigate and where appropriate, put things right. After all it’s in patients’ interest. Wrong. This is not how the NHS currently works in many hospitals, care homes, institutions and clinics.
Staff do need to raise concerns – why? Because, like in most walks of life, there will be situations which needs special attention. There could be issues, such as potential fraud, mismanagement of resources, safety issues, staff training issues which can relate to both staff and patients. There are of course, numerous more examples. As staff we have it ‘ingrained’ into us as part of our training about having ‘duty of care’ and reporting anything that we feel needs attention. Doing otherwise and ignoring would constitute neglect. Staff being able to safely raise concerns is vital to patient safety.
One of the earliest NHS whistleblower who has been in the public domain has been Steve Bolsin, who first raised concerns over 20 years ago about children’s heart surgery at Bristol. He is now based in Australia. Since then not much has changed. Whistleblowers’ raised concerns are still ignored despite in many cases, having extensive evidences. Whistleblowers are subsequently victimised and persecuted and find themselves being accused with false counter allegations, despite in most cases there are lack of evidence of any wrong doing. In some cases hyped up to be more serious than it really is as in David Drew, who was accused of quoting bible in a meeting. This was deemed to be more serious than the concerns he had raised about child safety, which led to the death of a child due to arrogance and neglect.
Whistleblowers within NHS come from a wide range of occupation, which include Chief Executives, such as Gary Walker and John Watkinson. Both raised patient safety concerns and both lost their jobs.
Since becoming a whistleblower myself, nearly 5 years ago and developing my website, I have been in contact with numerous whistleblowers. Many of the cases are devastating where the whistleblower have suffered gross injustice. Many cases are truly heartbreaking.
One example, is that of a senior staff member who was raised concerns about dealings with child abuse. She has now not only been left without a job, she is homeless, and now lives in a friend’s garage and depends on provisions from food bank. Another is a single mother of 2, who also now has to rely on food bank and in due time may have her home repossessed. I too, am likely to lose my home soon whilst suffering cancer.
My case is perfectly summarised by Courtesy of NHS Mess @NH_Mess
Many of the whistlebowers face years of stress. Many end up having counselling or have nervous breakdowns. It has profound effect on close family & friends. Many relationships breakdown under stress as in reported cases of Edwin Jesudason and Gary Walker. Sangita, Raj Mattu’s wife on Channel 4 news said that they have been unable to have children due to ongoing legal battle and stress. There are also known whistleblowers who have committed suicide or have suffered mental breakdowns, as it all got too much for them. Their health take a toll. David Drew has suffered serious health problems, despite leading a healthy life. I have developed cancer, which numerous consultants believe is stress related.
There are very few known whistleblowers who have faced legal battle with their trust and have return to their workplace. I only know of one – Ramon Niekrash. However, he was left with legal fees of £120,000. Nearly all NHS whistleblowers, once dismissed, never return to their workplace. Very few continue to work in their field of expertise and even fewer manage to secure permanent posts. This is because of existence of blacklisting within the NHS. There is of course in addition gradual loss of skills once being unemployed. For many, only option is to leave the country and look for work in other parts of the world, such as Steve Bolsin.
So why do whistleblower’s bother to raise concerns or blow the whistle where not only are their concerns on the whole are ignored but their whole career is destroyed? Because on most occasions, they feel they are simply doing their job and are confident that their concerns will be sorted. Very few give a thought for their own safety as naively it never enters their head. However, having made an example of a whistleblower, trusts send out a strong message to other potential whistleblowers. Many are deterred from speaking up. This means that patient’s safety is compromised. If staff are too scared to speak up, it means that the risk factor is never investigated, let alone sorted.
So why are whistleblowers persecuted? In some cases by bringing to light the concerns could be a source of embarrassment to senior managers and could attract unwanted publicity. It could be a costly expense to fix and organisations may have targets they have to meet. Individuals within the organisation may have vested interest for example, as in cases of theft and fraud. It could also be due to basic retaliation of ‘I go or they go’ (this could be due to the whistleblower having raised concerns about them) or it could be that individuals are looking out for their colleagues who have done wrong, but have a strong position in their organisation.
Watch the dynamics of whistleblowing
Those spending public money covering up their wrongdoing have been getting away with it for over 15 years, since Public Interest Disclosure Act, PIDA, was introduced.
The Chief Executive, The Medical Director and The HR Director are ultimately responsible within Trusts to ensure that victimisation of whistleblower does not happen, but unfortunately far too often, they are part of the victimisation. Trusts are given easy access to legal funds which are paid by taxpaying public. These funds are authorised by the Department of Health and paid out by The Treasury.
Ironically, huge sums of money which should have gone into patient care is used to fight and get rid of whistleblowers – the very people who care and want to protect the patients and the health service. It would be interesting to survey the tax paying public to have their views on their hard earned money is continually being wasted on getting rid of whistleblowers. After all, they are paying for this wastage. Raj Mattu’s case is a good example, where not only did Raj suffer for 13 years, but it has costed the tax payer £20m. Money which should have been used to benefit the patient. In addition, more recently, case of Arjuna Weerasinghe, where seven figure settlement is now being considered.
Of course, it isn’t just money that is being wasted, but there is also huge waste of expertise at all levels, which is being drained from the NHS. The very people who care what happens in the NHS are the very people who are being removed and having their lives destroyed.
Why is this allowed to happen? Nearly all whistleblowers once they realise they are in trouble and are in need of urgent help their first port of call is to their unions. I have yet to meet a whistleblower who has been successfully supported by their union throughout the ordeal. I am not sure whether this is due to lack of understanding, lack of money, or simply they want to remain in good terms with individual organisations. Strange as it may seem, in some instances, unions have turned on their own members.
The next step for a whistleblower is to get legal advice. Some firms are happy to give free short advice over the phone. Consultations can be expensive but vary. Mine cost £398 per hour, four years ago. Often with no money, whistleblowers setlle for ‘no win, no fee’ arrangement. However, legal costs escalate at an alarming rate. Many turn to policies in their home insurance. This has certainly saved the day for many, such as Anabelle (Loo) Blackburn and Jennie Fecitt. However, unfortunately some, such as mine, there was an opt-out clause, where if you belonged to a union, your policy will not be covered. My legal fees had escalated to £130,000 on a ‘no win – no fee’ basis.
Nearly all whistleblowers I have come across had written to both Care Quality Commission and Department of Health for help. Virtually all have been left without help, despite having strong evidence. Nearly all have received a standard reply, which stated that they could not get involved due to ongoing legal case. So, where is a whistleblower to go when they find themselves in deep water? Nowehere, is the answer. No one will intervene or inspect surroundings of the case. Cases are frequently dragged out over years before reaching a settlement. This is often deliberate attempt by Trusts who have endless legal funds to drain any funds that the whistleblower may have, to reach a settlement in their desperation. Also, if they are on ‘no win –no fee’ arrangement, they often have to settle out of court with substandard pay-outs, often just enough to cover their huge legal expense.
In contrast, trusts and organisations are fully supported with advice and access to funds by The Department of Health. So, stating that either Department of Health or Care Quality Commission cannot get involved in their response to a whistleblower is untrue. They do get involved, but simply not on the side of the whistleblower.
So, having suffered over the years and finally reaching some sort of settlement, you would think that there will be some help. No, is the answer. With career and any remote job prospects, livelihood, personal life and health destroyed, there is simply no help. Even when proven to be a whistleblower by courts, there is no help. Whistleblowers are left abandoned. So, who should be there to ensure that whistleblowers, responsible members of our society are taken care of? Fingers currently point to Jeremy Hunt and The Department of Health. After all they are ultimately responsible for the running of the health service. To say that they ‘cannot get involved’ is no longer acceptable. Hunt has instigated review into NHS whistleblowing led by Sir Robert Francis QC. Results and recommendations of which are due in November. This is a step forward. However, any recommendations made will need to be effectively implemented and not ignored.
I have yet to hear of any senior managers, directors, executives held to account for their treatment of whistleblowers. Yet, nearly all NHS organisations now have whistleblowing policies. Clearly, written policies are not worth the paper they are written on if no one acts on them. It needs a responsible governing body to take responsibility and ensure that all staff, patients and public for whom they are in charge have an in depth understanding, compassion, leadership and willingness to drive this forward. Until this happens, lives of both patients and staff will continue to be destroyed.
For more information and articles on whistleblowing visit sharmilachowdhury.com
‘No doctor should be untouchable’ Peter Wilmshurst
BMJ 2013;346:f2338 doi: 10.1136/bmj.f2338 (Published 19 April 2013)
PERSONAL VIEW
No doctor should be untouchable
Even very senior doctors must be subject to the same codes of conduct, and to the same sanctions when they are breached, says seasoned whistleblower Peter Wilmshurst
Peter Wilmshurst honorary consultant cardiologist, University Hospital of North Staffordshire, Stoke on Trent ST4 6QG, UK
Allegations that Jimmy Savile sexually abused children and vulnerable hospital patients surfaced after his death, when he was no longer protected by the English defamation laws. These laws were designed to protect the wealthy and famous from allegations by poorer citizens by making it difficult and expensive to defend a defamation claim, even if you are telling the truth. Should we blame the cover-up entirely on the libel laws?
There were those in authority at the BBC (where Savile had star status), in hospitals where he had unprecedented access, and in the criminal justice system who had heard reports of his misconduct but failed to act. Victims were told that their testimony would count for little compared with the word of the television star and charity fundraiser. Savile was valuable to the organisations and his victims were not. Savile himself bragged that he was untouchable. Other organisations that have covered up misconduct include the Catholic church over child abuse by priests, and the South Yorkshire Police over their failings at the Hillsborough disaster. Organisations protect their members, and senior members are, like Savile, often powerful and untouchable. I believe, based on observation of the outcomes in several cases in which I have been involved, that the medical establishment is no different, with senior doctors being untouchable. Indeed, once, when I raised concerns at a meeting at the Department of Health about a senior doctor, I was even told that he was
“untouchable.” I know that over many years the General Medical Council had refused three times to investigate allegations about him from other doctors (not from me). On 23 November 2012, the Department of Health wrote to me that the current chief medical officer is unable to discuss the issue with me “due to pressure on her time.” Refusal to hear allegations will allow later denial of knowledge of them.
The GMC investigates serious allegations about doctors, but in my experience it will often refuse to investigate the most senior doctors.
I reported Clive Handler to the GMC for financial misconduct. When he appeared before the professional conduct committee, the chairman of the committee, Peter Richards, had to stand down from the hearing because, in his role as medical director of Handler’s hospital, Richards had agreed to conceal Handler’s misconduct from the GMC.1 2 The GMC refused requests from its own solicitors and from me to take action against Richards, who had clearly broken the GMC’s rules on reporting misconduct by other doctors. Richards, who held many senior positions, including chairman of the Council of Deans of UK Medical Schools and Faculties, returned to chair hearings at the GMC after Handler was suspended from the medical register. Senior managers at the Royal Brompton Hospital knew that over many years Professor Peter Collins had used qualifications he had not been awarded.1 2 They knew that he had obtained three posts using false qualifications and that he put them on his letters. The whistleblower was informed by letter from the chairman of the board of governors that unless he dropped the matter his career might suffer. I reported Collins to the GMC. The GMC informed me that no public hearing was required because they had accepted a private assurance from Collins that he would not use false qualifications again. In the few years before and after the GMC’s decision on Collins, seven more junior doctors faced public hearings for claiming qualifications they had not been awarded. Six (Rashid Rhalife-Rahme, Seth Atardo, Ashoka Prasad, Afolabi Ogunlesi, Abu Shafi, and
Ashutosh Jain) were removed from the medical register and one (Sahmin Pandor) received a reprimand.2 They differed from Collins (educated at Cambridge and St Thomas’) in many respects, including the fact that most had only once claimed qualifications they had not been awarded. The GMC does not allow a doctor to voluntarily remove his or her name from the medical register when he or she is under investigation. However, twice, when I reported heads of medical institutions to the GMC for concealing research misconduct within their institutions, the GMC informed me that, as a result of administrative errors, each had been allowed to remove their names voluntarily, so the GMC could not investigate my allegations.
Competing interests: I have read and understood the BMJ Group policy on declaration of interests and declare the following interests: I have defended three libel claims brought by a US medical device company, and I have reported several doctors to the GMC. Provenance and peer review: Not commissioned; not externally peer reviewed.Despite legislation meant to protect whistleblowers, I am aware that an NHS trust and a health authority spent more than £2.5m (€2.9m; $3.8m) in legal fees before getting a whistleblower (a junior doctor) to accept a legal settlement that included a gagging clause preventing him from revealing illegal activity by a senior doctor. A deanery was complicit in the victimisation of the trainee. Allowing for additional management time and the financial settlement with the doctor, the protection of a senior doctor probably cost the NHS more than £5m. If we are genuinely going to put patients first, then nobody, no matter how senior they are, can be untouchable. However, this will only happen when we have a cultural change in healthcare, with promotion of real openness and real protection for whistleblowers, plus reform of the English libel laws to provide a genuine public interest defence.
- Wilmshurst P. Dishonesty in medical research. Med Leg J 2007;75:3-12.
- Wilmshurst P. The General Medical Council—a personal view. Cardiology News Oct/Nov 2006;10:13-15.
Cite this as: BMJ 2013;346:f2338
© BMJ Publishing Group Ltd 2013
Jeremy Hunt: message to NHS staff on ‘Sign up to safety’ campaign
The Secretary of State for Health talks about how improving the safety and quality of care can reduce costs in the NHS.
Last week I visited Birmingham Children’s Hospital, where the staff are rightly proud of the quality and safety record they worked hard to achieve. They are leading the way in bringing the highest safety standards to paediatric care, and are ambassadors of the Sign up to Safety campaign.
BCH is one of over a 100 trusts that have joined the campaign – which aims to reduce avoidable harms by 50% and save 6,000 lives over the next three years.
The enthusiasm shown for Sign up to Safety is a remarkable testament to the ongoing commitment of the NHS to learn the lessons of the failings in care at Mid Staffs. I am delighted that so many trusts are on board, and I look forward to many more joining them to help make the NHS the safest healthcare system in the world. To join them click here: Sign up to Safety.
While visiting BCH, I spoke to staff about the value of safe care – not just for patients, but for the NHS too. I talked about how unsafe care is costing the NHS between £1bn and £2.5bn each year – money that could be invested in more front line staff, better training, better equipment and more time for you to care.
A poster and leaflet are now available for you to display in staff areas – highlighting the value of safe care and the potential savings that could be made and reinvested by reducing avoidable harms. Click here to download the poster and poster/ leaflet.
Of course, not all cases are avoidable, but poor care is expensive and wasteful. It’s down to all of us to prioritise safer care for patients.
I know that NHS staff work tirelessly to ensure the safety and welfare of their patients, but it is important for patients to know the steps they can take to keep themselves safe.
Information and advice is now available in the form of an airline-style safety advice video and information card, which hospital patients can use. The video has already been piloted with positive feedback from patients and staff. You can view the video here, and share it with your patients. It can be incorporated into your hospital’s website so patients can watch it before they come into hospital, and hospitals with the Hospedia patient media system will be able to show it to patients once in hospital.
There is so much excellent work being done across the NHS on improving patient safety and compassionate care which is making a real difference for patients. The respected Commonwealth Fund already rates the NHS as leading the world in patient safety, and I know that the NHS is full of organisations and individuals ambitious to do more. They tell me that being the best healthcare system for safety is not enough for them. They want patients to have an NHS that is the first healthcare system in the world with the same safety standards as the airline industry. What I have seen and heard this week gives me real confidence that we are now on that journey. Thank you for your continued commitment to keeping patients at the heart of all you do.
Whistleblowing heart surgeon at Welsh hospital is suspended on full pay for two years costing the NHS more than £500,000 – while country faces ‘cardiac care crisis’
- Peter O’Keefe was sent on ‘gardening leave’ in April 2012
- He is still being paid his £94,000 and the hospital in Cardiff has had to recruit a locum consultant to cover Mr O’Keefe
- The total cost to the NHS is thought to be more than £500,000 as a result
- A formal investigation was launched by health bosses in Wales but a barrister appointed to chair the case was taken ill earlier this year
- Health chiefs declined to comment on the details of the case against Mr O’Keefe but said it was not to do with the standard of care he provided
Heart surgeon Peter O’Keefe has been suspended on full pay for more than two years, at a cost to the NHS of £250,000
A heart surgeon has been suspended on full pay for two-and-a-half years at a cost to the taxpayer of up to £500,000 while he faces bullying allegations.
Consultant Peter O’Keefe, 49, has been on ‘gardening leave’ since April 2012 amid fears he has been targeted as a whistleblower for raising concerns about patient care.
The NHS in Wales is continuing to meet his salary of around £95,000 a year while having to pay a similar sum to another surgeon filling his role.
Mr O’Keefe was suspended from the University Hospital of Wales in Cardiff after being accused of bullying junior colleagues.
But 18 months previously he voiced concerns about the treatment of a patient who suffered serious brain damage. His intervention resulted in a critical report into safety failings.
Mr O’Keefe has been prevented from working at a time when his hospital has been heavily criticised for lengthy waiting lists for cardiac procedures.
The Conservatives accused health bosses of wasting money that could be spent on treating patients by ‘dithering’ over the disciplinary hearing – the latest in a series of scandals to hit the Labour-run Welsh NHS.
Cardiff and Vale University Health Board denies there is any link between the surgeon’s suspension and his earlier complaint about care standards.
A friend of the cardiothoracic surgeon said Mr O’Keefe suspects he was victimised for speaking out.
One source told The Sunday Times: ‘There was annoyance on the intensive care unit that he had reported the matter.’
But a spokesman at the Cardiff and Vale University Health Board told MailOnline, that is ‘absolutely’ not the case.
‘We absolutely reject the suggestion that the suspension of the surgeon in question is in any way related to any concerns he may have expressed about the care of patients,’ he said.
‘The process of suspending a consultant is not one that this health board enters into lightly.’
His case was highlighted by the Conservative opposition in the Welsh Assembly yesterday, as an example of waste in the NHS.
Shadow Health Minister Darren Millar said: ‘When serious allegations are made against any member of NHS staff, it is right that such claims are thoroughly investigated.
‘But there is no reason why it should take over two and a half years.
‘Against a backdrop of a crisis in cardiac care that has seen Welsh patients sent to Bristol for treatment because waiting times were so severe, the Welsh NHS cannot afford to have specialist surgeons suspended for two and a half years on full pay.

The 46-year-old was sent on ‘gardening leave’ in April 2012 and a formal investigation was launched by health bosses at the University Hospital of Wales in Cardiff, pictured. While they declined to comment on the allegations against Mr O’Keefe they said the case has nothing to do with the standard of his work
A barrister appointed to chair the case was taken ill earlier this year, causing a delay. The hospital has been forced to employ a locum consultant to cover Mr O’Keefe’s work, at a cost thought to be close to the £94,000 salary the heart surgeon, pictured, is paid
‘The Welsh NHS is reeling from Labour’s legacy of record-breaking cuts.
‘Yet a health board which last year had its accounts qualified for breaching its spending limits can afford to pay a senior surgeon a near-six-figure salary while suspended and pay similar salaries to locums to cover his workload.
‘Health chiefs must end their dithering approach which is wasting NHS cash that could be spent improving patient care and reducing cardiac waiting times.’
Dr Richard Lewis, Welsh Secretary of the British Medical Association, said: ‘I can’t comment on the circumstances of this particular case, but long suspensions are never good for the individual concerned or for the health service.
‘If an individual is able to return to work after a disciplinary hearing, they will require retraining after a long period of absence.’
Dr Graham Shortland, the medical director for Cardiff and Vale University Health Board, said: ‘We do not take disciplinary steps lightly, but believe that when serious allegations are made the University Health Board has a duty to patients, staff and the people we serve to investigate such allegations thoroughly.
‘We can confirm that a surgeon has been suspended since April 2012. We have been following the Welsh Government’s disciplinary procedure in order to ensure there is a full and fair investigation.
‘Unfortunately, through no fault of either party, the process which has already taken far too long, has been held up. However, we hope to be able to secure a way forward in the next few weeks.
‘Due to the legal and confidential nature of such issues we are unable to say anything further.
‘We would like to reassure the public that the health board is doing all it can to bring this matter to a swift resolution which is in the best interests of all involved.’
The board confirmed that Mr O’Keefe’s surgical work was being covered on a locum basis to minimise delays for patients.
Locum costs are on the consultant pay scale between £72,927 and £94,679.
Mr O’Keefe, who qualified as a doctor in 1987, did not wish to comment.
Parents’ long wait for truth on baby’s death may be over
The Guardian, Tuesday 14 October 2014
Changes in how health ombudsman operates mean historic cases such as the death of Anne and Graeme Dixon’s daughter could now be investigated

Anne and Graeme Dixon have spent the past 13 years investigating the death of their 11-month-old daughter, Elizabeth, and the treatment she received after her birth. Now, due to recent changes in the way the parliamentary and health service ombudsman (PHSO) works, they believe they could be a step closer to finding some answers.
Elizabeth was born eight weeks early, in 2000, in Frimley Park hospital in Surrey. Immediately after birth, her blood pressure began to rise but was left untreated until she was transferred to Great Ormond Street hospital some two weeks later. By that time, Elizabeth had suffered severe brain damage. It was another 10 months before the Dixons were able to take their daughter home. Then, just days before her first birthday, Elizabeth died during the night, after her breathing tube became blocked when an agency nurse failed to maintain it.
In 2005, the nurse was struck off the nursing register and an inquest into Elizabeth’s death was held in 2009. But the Dixons, from Fleet in Hampshire, believed many questions remained unanswered and continued their own investigations. Last year, after new evidence was uncovered by the couple, Frimley Park hospital eventually commissioned an independent review into Elizabeth’s care in the days following her birth. The report found that hospital staff failed to monitor or treat Elizabeth’s high blood pressure and concluded it was overwhelmingly likely that Elizabeth’s brain damage was caused by uncontrolled severe hypertension.
“It was a bitter irony that we only discovered the true cause of our daughter’s disability while investigating her death ourselves,” Anne Dixon says. “It had taken years of sheer determination to get our evidence together and all that time, in the back of our minds, we were wondering if other babies were at risk.”
The hospital later apologised for Elizabeth’s poor care and the family approached the Care Quality Commission (CQC) with the findings of the report. In the summer of this year, after many discussions with the Dixons, the CQC pledged to work in partnership with NHS England to establish an independent investigation panel to look into Elizabeth’s case. But in August, NHS England backed out of the investigation, meaning the CQC would only be able to carry out a “thematic review” to look at the issues raised by Elizabeth’s death, as they can not look into historic, individual cases of poor care.
The case has highlighted how difficult it can be for families with historic complaints to have their concerns investigated. The CQC chief executive, David Behan, has expressed concern over what he describes as a “gap in the system” when it comes to such cases. Speaking at a CQC board meeting in September, Behan said: “There are issues surrounding how old a case is. Five years ago, I think there would have been a different response to saying a complaint is time expired, but since cases like Hillsborough, Rochdale and Rotherham, I don’t think you can say that. That argument has now gone in public services.”
In the last few weeks, the Dixons have been in contact with the PHSO about the possibility of it investigating Elizabeth’s case. The PHSO, which was set up to investigate complaints about health service providers and government departments, can provide a final, independent and impartial adjudication.
Until recently, it was rare that it took on historic cases. But as part of major changes to the way it works, older complaints could now be reviewed more regularly. By lowering the threshold for investigating cases from only investigating if the evidence showed it was likely to uphold the complaint, to now doing so if there is a case to answer, and by shortening assessment times, hundreds more cases are being considered. Between April 2013 and March 2014 figures show the total number of investigations soared to 2,199, compared to just 384 the previous year.
Although the PHSO says it won’t comment on specific cases, the ombudsman, Julie Mellor, says the changes include a shift to using their discretion more positively to help more people. “For serious cases that come to us outside the normal 12-month period specified in law, we will now positively consider whether an effective investigation is possible given the passage of time. Where we judge it possible, we will generally investigate.”
The Dixons hope the changes could finally bring them answers about their daughter’s case. “Many complaints only become historic because families have battled for years to find evidence to put forward. As a consequence, opportunities to improve safety of care in the NHS are wasted,” Graeme Dixon says. “Our hope now, is that the possible involvement of the PHSO in our case, together with the thematic review by the CQC will raise awareness of the issues surrounding infant hypertension and tracheostomy care in the community, and ultimately save the lives of other children.
Whistleblower ‘bullied by bosses’
30 September, 2014 |
West London Mental Health Trust has accused a whistleblower of constructing “conspiracy theories” during an employment tribunal in which it faces bullying claims.
The former employee, psychologist Dr Hayley Dare, has alleged she was targeted with a threatening poison pen letter just weeks after raising concerns about a culture of poor practice within the forensic clinical unit at the trust.
The letter, as described in Dr Dare’s witness statement, urged her to withdraw her claims, warning her “you cannot beat us” and “how hard it will be on your children if you are unemployed”.
Dr Dare was also the target of alleged bullying by two of her bosses, causing her to suffer depression, anxiety and suicidal thoughts, Watford Employment Tribunal heard.
She has launched a case against the trust for detriment she claims she suffered as a result of her whistleblowing in early 2013.
The trust is the one of the largest in the country and is responsible for high security hospital Broadmoor as well as low secure units and local services.
Speaking of her whistleblowing, she told the tribunal: “I went to the chief executive to make some serious allegations against clinical staff and senior managers who had breached their duty of care in terms of patient care and staff welfare that could have led to a patient death.
“This was never about an individual; this was about poor patient care and bullying from a culture within the forensic clinical service unit.”
She added that the treatment she suffered was a direct result of the trust failing to investigate her claims properly.
Dr Dare was given nearly six months off work as a result of her distress but claimed the bullying continued after she returned and her work was undermined by colleagues.
But Ian Scott, representing the trust, accused Dr Dare of enjoying “conspiracy theories” and denied that her colleagues were in a “cohort” against her.
He added that the trust has provided her with support to help her return to her job.
Dr Dare started working for the Trust in 2000 and was appointed clinical head of the women’s forensic directorate in 2011.
The tribunal is due to give its ruling on November 10.
My Story – Noel Finn, Serco whistleblower
 Noel Finn
Noel Finn
I have experience of raising concerns in the NHS and private providers of NHS services. I am not represented by Patients First or any other organisation.
My experience in NHS was whilst employed as a service manager from 2006-2010, and involved many concerns which were raised over 3 years including: inaccurate reporting of performance data; fraudulent activity of medical staff; experiences of bullying; dangerous working environment; inadequate service cover and staffing levels.
These concerns were raised as I became aware of them and reported directly to my line managers, senior managers and service leads as appropriate; through supervision, various forums and meetings.
Most concerns were not addressed or resolved satisfactorily i.e. the problems remained or created another problem, therefore I continued to pursue issues in an effort to seek resolution.
Eventually, I became more isolated and managers and colleagues alienated me. During the same period I was tasked with improving the standards and performance of the community services I managed, which involved performance managing some of the staff and implementing change. Where performance management was required I ensured that I sought advice and support from HR throughout, and made reasonable adjustments for people to adapt to change. However, on two separate occasions different staff members raised allegations of bullying against me in response to such management. Both allegations proved unfounded, however on both occasions I was ‘operationally suspended’ i.e. temporarily removed from my role whilst the investigation was held. None of the staff members concerned faced any disciplinary actions following false allegations, and my managers, investigators and HR ignored my concerns that I was being victimised. On commencement of the second allegation I also raised a grievance which included all of my concerns to that date, and at that point the investigation was escalated to a disciplinary hearing. The organisation did not follow ACAS guidance and tried to pursue the disciplinary before the grievance, however then arranged to hold the grievance and the disciplinary on the same day.
On this day the disciplinary was immediately thrown out without question, and despite a massive file of my concerns to that date, these were given scant regard although my grievance was partially upheld. However, I was never allowed to return to my role as service manager on the grounds that I needed time away to heal from the experience. Following the outcome of my grievance I questioned the outcome, reinforcing that I needed to return to the role I had held, however I was told by the director that if I insisted on this, the disciplinary investigation would be resumed. I was promised that at the least, I would be able to return to meet with the team to be vindicated, but this did not happen and I later learned that the allegers both received apologies from the director for the experience they had suffered, and an implication that my being moved from the team was as some form of disciplinary action.
I was moved to a team to be managed by someone who was known to have had previous allegations of bullying against them, who then directly bullied me, following which I resigned.
Whilst working my notice, I also raised my concerns in writing to the CEO and other senior directors, but received no acknowledgement or response.
I had support from an RCN officer during the disciplinary and grievance and that was very helpful. I was then passed to the RCN legal team for assessment of my case after I resigned and a case was put forward for constructive dismissal as a result of whistleblowing and an application made to the employment tribunal (ET). This was the first time that I saw my actions as ‘whistleblowing’. The whistleblowing element was removed from the case early on by the judge due to a timing issue. The case reached a conclusion before tribunal, but I was ‘gagged’ from speaking of my experience.
I wrote to the CQC to escalate some of the issues I had raised as they still had not been addressed. One concern regarding dangerous working premises, when raised by the CQC led to the Trust immediately removing the team from the building and relocating them – I had raised the same concern over a period of three years and no action had been taken in that time. The CQC also wrote to me to advise that other concerns had been put to the CEO who had given assurance that issues did not remain but that evidence would be sought at the next inspection. I was also advised to take my concerns to the parliamentary ombudsman, which I later learned was inappropriate as they act only on behalf of patients. I also received an apology from the Trust which is subject to confidentiality outside my immediate family.
My second experience was whilst working for Serco Healthcare at Yarlswood Immigration Removal Centre.
Following my experience in the NHS I was unsuccessful in applying for numerous jobs in the NHS, initially at the same level (service manager) as I had been employed, but then at entry level and ‘bank’ roles, turning also to private healthcare. Eventually after a period of almost 2 years I commenced employment as a bank nurse at Yarlswood in January 2012.
After a few weeks I was asked to take up the post of Mental Health Lead-tasked with developing mental health pathways on a 3 day per week contract.
I quickly identified concerning mental health issues which needed addressing. Mostly acute in nature and related to risk – i.e. suicide and self-harm. I also identified that officers did not have relevant training to manage these risks and some had negative attitudes towards these behaviours and residents.
In March 2012 the role increased to 4 days per week due to the increased demands.
From the start I fed back all my findings and concerns to operational and healthcare managers and made suggestions on how these could be addressed. I also raised concerns around a lack of clinical supervision for healthcare staff.
I also uncovered issues with access to emergency NHS mental health services for residents.
The healthcare manager suggested I put my concerns into a business plan for consideration. In completing this I researched previous reports and inspections into Yarlswood including HMIP 2011, IMB 2010, and Bedford needs assessment and found the same concerns had been raised before. I also found that some policies and processes were not being implemented appropriately. The business plan included all of my concerns and findings, and different suggestions for change based on existing models of mental health care provision in similar populations. I made it clear within the business plan that the status quo could not remain as it was not sufficient to address the needs and safety of residents.
I sent the business plan to the healthcare contract manager on 1st October 2012. Following this the manager made it clear they were not happy with the plan and began to act with increasing hostility and began to bully me: making increasing demands on my work with the prime concern of fulfilling contract obligations; being increasingly critical of my work; making a false accusation of shouting against me; and physically pushing past me aggressively on one occasion.
Eventually I requested a reduction in my hours back to 3 days per week as the bullying was intolerable. In response the manager said that I would no longer be mental health lead and that my role would be completed by a different mental health nurse each day. I expressed my concern that this undermined the service and did not address any of the issues I had raised.
I reported the incidents of bullying and escalated my concerns to the regional manager. A grievance was formally raised on my behalf on 1st November 2012, whilst I was on leave.
I returned to work on 5th November 2012 and was immediately suspended by the Centre manager, for ‘failing to follow the instructions of healthcare management’. I was never given any detail of what I had failed to do, and never received any detail of the investigation despite it being progressed to a hearing in January 2013. The terms of reference were also very vague and indicated that there was no evidence to support my alleged misconduct. I was also instructed to contact a named manager before 10am on each day that I would normally be on duty. Serco never followed ACAS guidelines or employment law with regards to the whole investigation as it continued despite my grievance never being concluded.
I wrote to all managers to say that I considered my suspension to be a direct result of my raising concerns, but this was ignored. I also raised my concerns, and provided written statements during each of my meetings with investigators but was told that it was not the appropriate venue to address them.
The initial grievance outcome was appealed based on it being unfair due to my suspension; that it had many inconsistencies; that it was inappropriately handled (both the grievance and disciplinary were overseen by the same manager); and that my concern that the suspension was in response to me raising concerns had not been addressed.
The appeal process was initiated under another director, but was never concluded. The disciplinary hearing was put on hold only after the intervention of the RCN rep. Arrangements were made for me to enter Yarlswood under supervision to access evidence in support of my grievance and my claims that I had ‘whistleblown’, but this was cancelled at the last minute.
As no progress was made and the concerns I had were still not being addressed, I escalated all of my concerns to the then CEO of Serco Chris Hyman, and further raised to Valerie Michie, Serco MD.
Throughout my suspension I was supported by an RCN Rep who was very supportive.
A senior director was tasked to help resolve my concerns. They arranged a confidential meeting for me, my union rep and a member of Serco’s legal counsel. It was agreed that an investigation would be held into the concerns to be completed within 6 weeks, and that I would be interviewed as part of this. Terms of reference for the investigation were agreed at the meeting, but were later diluted so that they only looked at contractual obligations.
Myself and the RCN rep recommended that Serco report my concerns to CQC and have them involved in the investigation. However, the counsel said they contacted CQC informally who advised an internal investigation was sufficient.
Serco subsequently nominated their own external investigator, but I was never interviewed.
It was also agreed that the senior director would look into my disciplinary and agreed that I could stop reporting to the named manager by telephone on my normal days of duty.
Initially the director asserted the validity of the disciplinary. When I challenged this quoting the evidence, the suspension was immediately lifted and the investigation was dropped without explanation.
A meeting was then arranged with me, my union rep and a senior HR director to resolve my employment issues. My union rep and I stated that issues including the grievance should be resolved before my return to employment. However, both directors disagreed and instead offered 3 options – return to Yarlswood, redeployment or leaving the company. Details of the first 2 offers were provided, but were deemed inappropriate. Therefore I asked for further details on the 3rd option as this was not provided at the time.
As the investigation into my concerns had not started and Serco refused to inform CQC, my concerns were escalated to Bedford CCG by the RCN on my behalf, stating that I was also available to talk to them for further detail.
As the commissioning arrangements for Healthcare at Yarlswood were in transition my concerns were forwarded to NHS England, who then spoke to the manager who had bullied me; Home office and the CQC. However, the concerns were not disclosed in detail and I was never contacted. HMIP and CQC both later performed inspections and did not record that disclosures were made and therefore did not look at the issues. Through a FOI request I later learned that CQC were not given any detail of the disclosures from Serco despite asking for them.
At the 6 week deadline the investigation had still not been started, and I was forced to resign my post.
My case was then referred to the RCN legal team. They advised that whilst it was clear that I had whistleblown and suffered detriment, they would not argue for constructive dismissal or apply to ET as they would not take the financial risk. Their analysis on the success of my case was flawed. They advised to negotiate a settlement. I expressed concern from the outset that Serco’s actions against me were a serious concern for the nursing profession and therefore in the RCN’s and public interest to address, but they refused to pursue due to constraints on funding. I proceeded therefore with the advice but insisted on an open apology as part of the remedy.
Twice the legal officer made serious errors and resolution was still not in sight as the deadline for application to ET approached which the RCN still refused to support, therefore I withdrew from the RCN and sought independent legal advice.
My new legal team agreed to make an application to ET and advised me to apply for legal fees under my household cover or ask RCN to cover my expenses. Neither option was successful so I had to self-fund.
During the whole experience I became very depressed and reluctantly started antidepressants in late 2013. At the request of Serco and my legal team I was seen by an independent psychiatrist for assessment. The psychiatrist suggested I had suffered Occupational injustice, and that I was not recovered sufficiently to return to a clinical role, he also suggested that moving into an unskilled role may be demeaning, therefore recovery was difficult to determine.
I was subjected to additional stressors through this process and continued expenses when I expected the case to be resolved. The case was eventually concluded over a year after resignation and I have received an open apology from Serco which recognises that the action taken against me was as a result of raising concerns, in the public interest, and was inappropriate.
Main problems were that people consistently did not listen or even acknowledge what I was saying, and did not act. In both experiences people made judgements about me as a troublemaker and for managers it seemed the easiest way to address problems was to get rid of me, anything else was too complicated.
There seemed to be a stronger culture of achieving targets and my concerns seemed to get in the way of achieving those.
In both experiences, colleagues often quietly agreed with my concerns but refused to speak out in fear of reprisals.
RCN legal team I believe have a conflict of interest with regards to nursing as their financial constraints prevent the public interest being served. The ET is not a fit place for whistleblowing as it is meant to represent individual employment issues and not the public interest. Timing issues should not be relevant to whistleblowing. Whistleblowers are not experts in employment law but healthcare companies have HR and legal teams on hand to advise at every opportunity meaning they have the upper hand. Finances also put employees at a disadvantage and thanks to Mr Vince Cable, the very individuals, who need to have a voice are unable to do so due to cost pressures, unemployment and having to pay for Employment Tribunals. On the ET application the new ‘whistleblowing box’ was ticked but the information was not raised to regulators, when I called the local Employment Tribunal office they did not even know who the CQC or HMIP were, this was shocking as the raised concerns need to be forwarded onto them. To this day I am still not aware if this has been done.
Regulators and responsible bodies failed consistently and more often took the assurances of organisations at face value rather than going to the source or exploring assertively in greater detail.
The experiences I had could be likened to abuse, however I think this is not at all appreciated or acknowledged anywhere and is not possible to resolve via ET.
I also submitted evidence to the Healthcare select committee and the Home affairs Select committee and have received no response or acknowledgement.
I believe the fact that the issues I raised related to mental health and latterly also immigrants, meant that they were less likely to be addressed as less priority or attention is given to these areas, and the present government does not make it any easier for these groups of people.
There should be a duty for all NHS (including commissioned providers) to report all concerns openly and for these to be taken to the board as the first step for oversight, assurance and accountability.
The CQC should have an independent element which is solely responsible for addressing whistleblowing concerns to ensure quality this includes involvement with other providers such as NHS England.
Whistleblowing detriments should not be taken through ET’s and should not be sectioned off into mild, moderate and severe pay-outs, this is nonsense; the detriment is a subjective thing, you can’t measure one against the other, people react and cope differently. It should have a separate process to ensure that public interests are not kept secret and any organisation found to have acted inappropriately against whistleblowers should be put in front of a public committee for scrutiny.
Apology from Serco after 3 years:
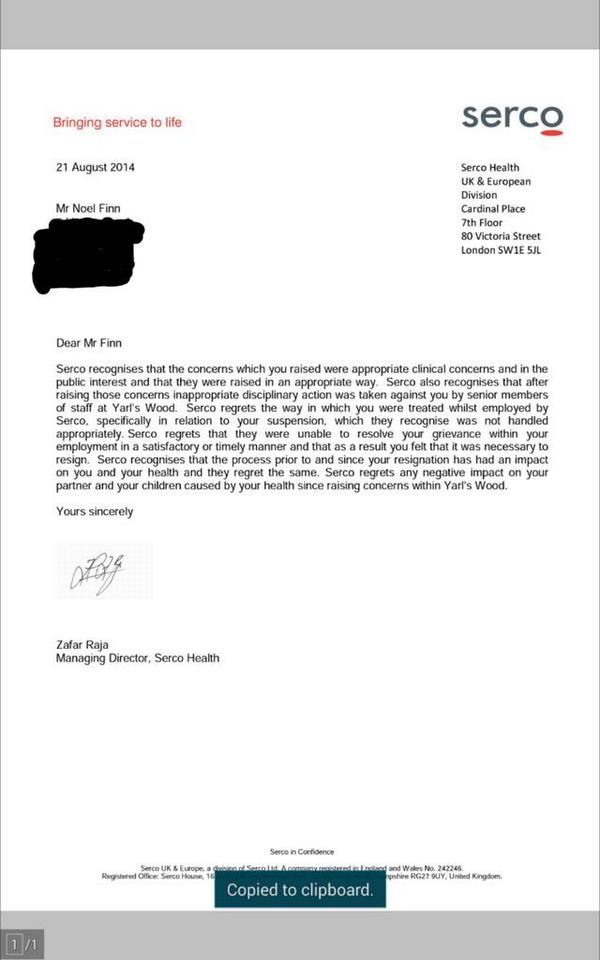
‘I have not been formally interviewed by any authorities to date, and despite an apology on both account on whistleblowing no one from CQC HMIP and CCG NHS England Monitor had interviewed me the assessment of Yarlswood in 2013 some 4 week after i resigned was reported to be fit and well, yet CQC ort HMIP never interviewed me despite knowing about the whistleblowing, furthermore they refused to peruse the document from Serco and myself . The CQC board had refused to talk with me directly, instead they passed my concerns down the line. I have recoding of these meeting not one had a clue about why they where meeting me. where is the accountability for the board they keep talking about it so freely, “transparent” its not, they need challenging.’
 Surgeon Shiban Ahmed accuses the health regulator of failing to prevent boys from having cruel and unsafe circumcisions, often carried out privately for Muslim children for non-medical reasons (Phil Tragen)
Surgeon Shiban Ahmed accuses the health regulator of failing to prevent boys from having cruel and unsafe circumcisions, often carried out privately for Muslim children for non-medical reasons (Phil Tragen)

